Background/Purpose: Cartilage damage impacts on patient disability in RA. The aims of this MRI study were to investigate cartilage damage over 3 years and determine predictive factors.
Methods: 38 RA patients and 22 controls were enrolled at t=0 (2009). After 3 years, clinical and MRI data were available in 28 patients and 15 controls. 3T MRI scans were scored for cartilage damage, bone erosion, synovitis and osteitis. A model was developed to predict cartilage damage from baseline parameters.
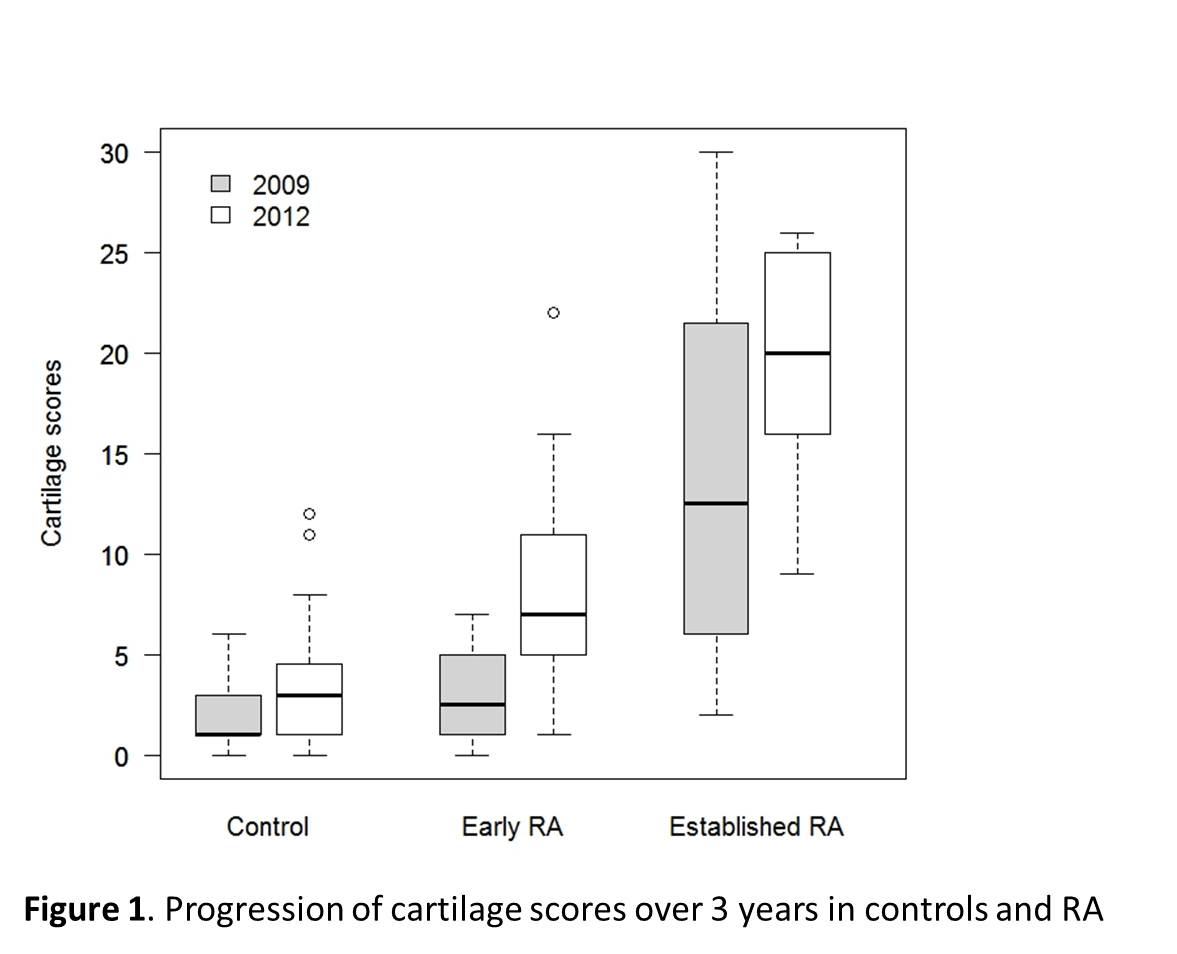
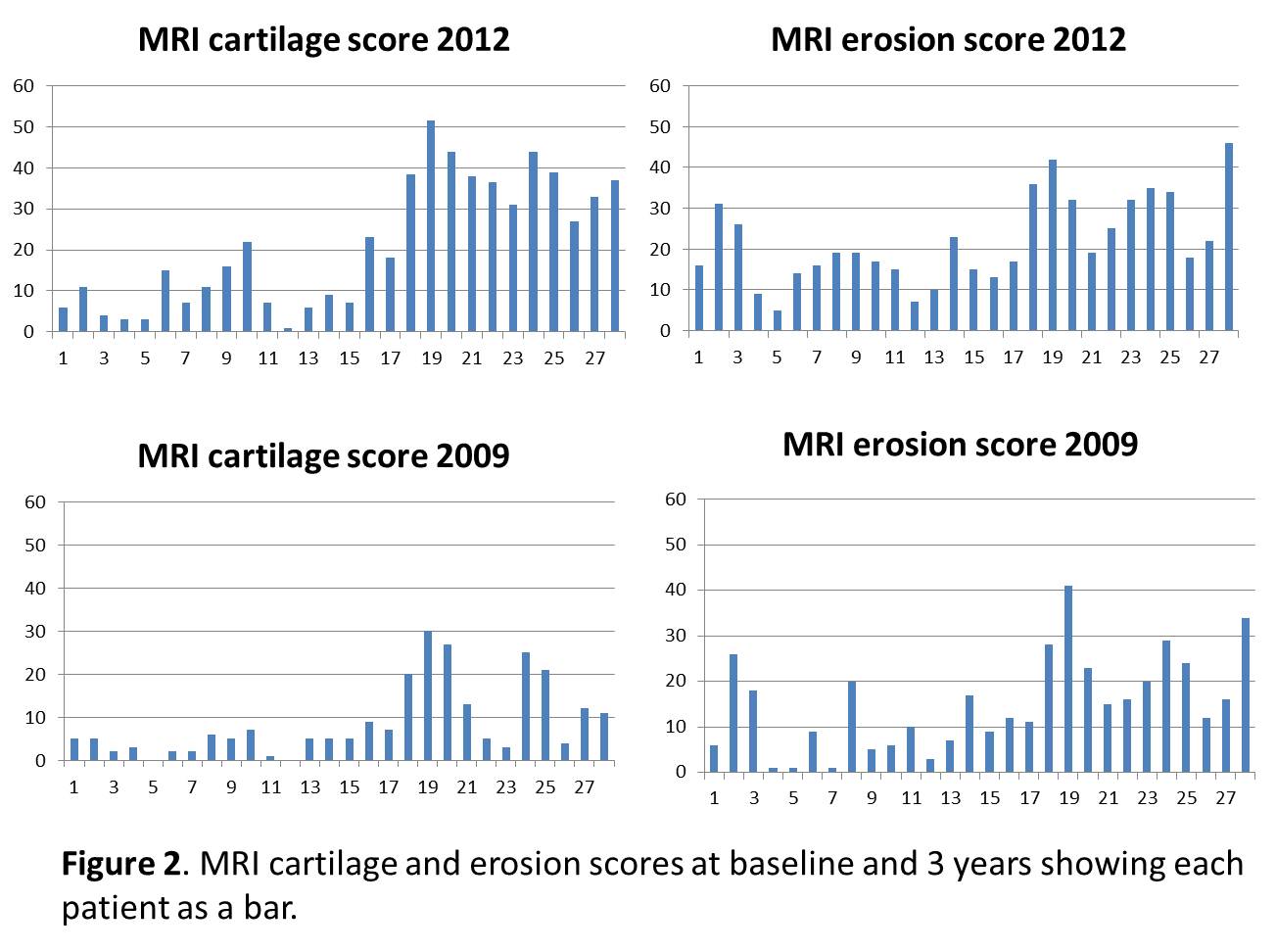
Results : Inter-reader reliability for the Auckland MRI cartilage score (AMRICS) (1) was high for status scores (ICC 0.90 [0.81-0.95]) and moderate for change scores (ICC 0.58 [0.24-0.77]). AMRICS scores were highly correlated with the OMERACT MRI joint space narrowing (jsn) and XR jsn scores (r =0.96, p<0.0001 and 0.80, p<0.0001 respectively). AMRICS change scores were greater for RA patients than controls (p = 0.06 and p = 0.04 for the 2 readers) (Figure 1). Using linear regression, the baseline MRI cartilage score was the strongest predictor of the 3 year MRI cartilage score but synovitis and osteitis scores were also predictive (R2 = 0.67, 0.37 and 0.39 respectively). Baseline radial osteitis predicted increased cartilage scores at the radiolunate and radioscaphoid joints, (p = 0.0001 and 0.0012 respectively) and synovitis at radioulnar, radiocarpal and intercarpal-carpometacarpal joints also influenced 3 year cartilage scores (p values of 0.001, 0.04 and 0.01 respectively). Using multiple linear regression with outcome of cartilage damage at 3 years the optimal model predicted 76% of the variance of the 3-year AMRICS (R2 = 0.76), the strongest component being the baseline cartilage score (R2 = 0.67). The baseline MRI erosion score was also predictive but to a lesser degree (R2 = 0.47). When the outcome of bone erosion score was used, the strongest predictor was baseline erosion score (R2 = 0.87, p < 0.0001), while baseline cartilage score was less predictive (R2 = 0.49, p = 0.01). These data would support the hypothesis that some patients favour one damage pathway over the other so that those who develop erosions tend to erode further (E-progressors) while those who damage cartilage continue preferentially in that manner (C-progressors) (Figure 2).
Conclusion : MRI cartilage damage progression is preceded by osteitis and synovitis but is most influenced by pre-existing cartilage damage suggesting primacy of the cartilage damage pathway in certain patients.
1) McQueen FM et al. Ann Rheum Dis 2010;69:1971-75.
ADDIN EN.REFLIST
Disclosure:
F. M. McQueen,
None;
A. McHaffie,
None;
A. Clarke,
None;
A. Lee,
None;
Q. Reeves,
Specialist Radiology and MRI,
3;
B. Curteis,
None;
N. Dalbeth,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-progression-of-cartilage-damage-in-rheumatoid-arthritis-a-three-year-prospective-3t-magnetic-resonance-imaging-study-examining-predictive-factors/