Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Lupus nephritis represents a severe manifestation of SLE and is associated with a risk of progression to end-stage kidney disease (ESKD) if untreated, leading to significant morbidity and high healthcare-related costs. Once patients with SLE reach ESKD and are initiated on renal replacement therapy (RRT), in the form of either dialysis or transplantation, it has previously been suggested that the disease becomes quiescent. However, our experience suggests that patients continue to exhibit active disease even after reaching ESKD. In this study we describe the temporal trends in disease activity for patients with SLE before and after ESKD from a single tertiary centre in South London. We also sought to identify whether there was a greater risk of ongoing disease activity across ethnic groups.
Methods: We conducted a retrospective observational study of consecutive adult patients with biopsy-proven lupus nephritis and ESKD who were under regular follow up in our unit from May 2004 to May 2023. Clinical electronic records were examined from the first point of entry until the end of the study period, transfer or death. Medication, SLE Disease Activity Index 2000 (SLEDAI-2K), dsDNA and complement levels were checked at 6-monthly intervals before and after the onset of ESKD. The primary outcome was disease activity using the SLEDAI-2K score, before and after the onset of ESKD. A SLEDAI-2K score ≤4 was considered low disease activity and >4 as active or flaring disease. Mean scores were compared using Wilcoxon’s signed-rank test.
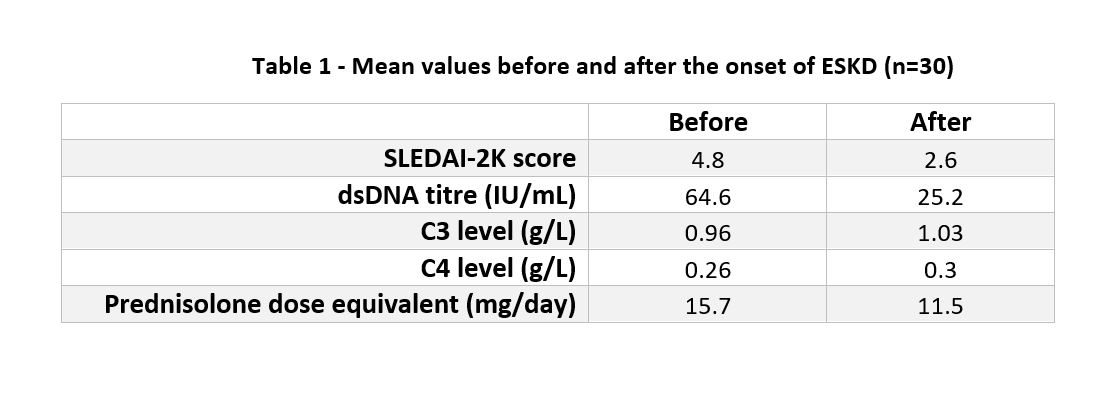
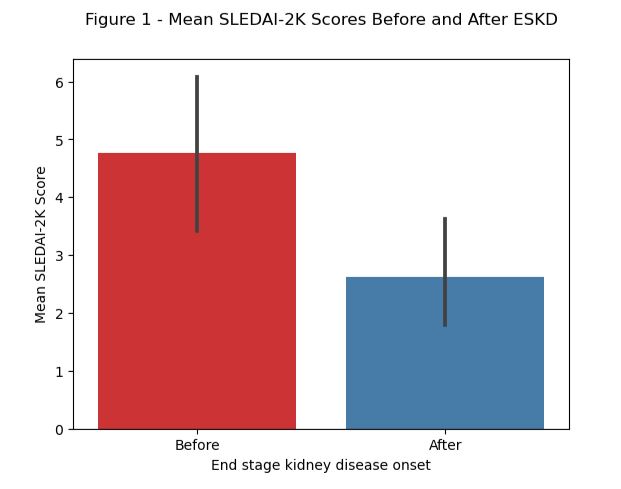
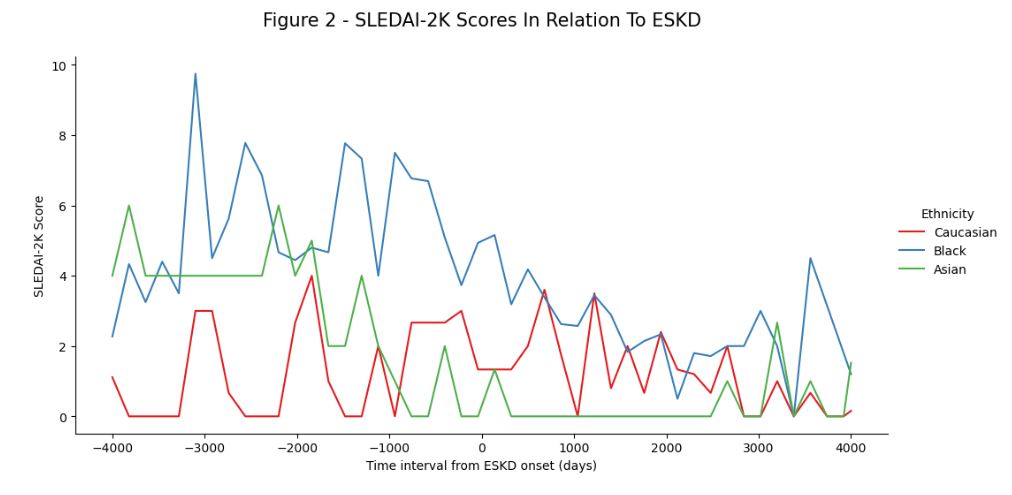
Results: Thirty patients were included (90% female, 67% of Black ethnicity, 20% Caucasian and 13% Asian) with a combined 369 years of follow up. The mean age at SLE diagnosis was 29 years (±11.7) and the mean interval from SLE diagnosis to ESKD was 11.8 years (±7.4). During this period 12 patients underwent renal transplantation, 18 patients received dialysis only and 7 patients died (4 with active SLE). SLEDAI-2K fell on average after the onset of ESKD although this did not reach statistical significance (Figures 1 and 2). Immunological markers of disease activity did appear to improve, as shown in Table 1. Of the 29 patients with >6 months of data after ESKD onset, 15 achieved consistently low disease activity within an average of 1.4 years (±2.5). However, 14 of the 29 patients exhibited active disease with an average time to flare of 2.6 years (±3.4). Nine of these 14 patients showed active disease within 18 months of ESKD onset and all were of Black ethnicity. Clinical manifestations after ESKD involved rashes, synovitis, serositis, myocarditis and neuropsychiatric involvement. Five patients ultimately required induction therapy with cyclophosphamide or rituximab.
Conclusion: Despite a fall in mean SLEDAI scores after the onset of ESKD, SLE disease activity persisted or flared in 48% of cases, often within 18 months of ESKD diagnosis. Our cohort were primarily of Black ethnicities, who are known to have more frequent and aggressive renal involvement. Our data contradicts the notion that SLE “burns out” in ESKD and supports a need for vigilance in the monitoring of patients with SLE and ESKD, particularly in those of Black ethnicities and within the first 18 months of RRT.
To cite this abstract in AMA style:
Patel S, Ghosh S, Sankara Narayanan R, Valisena L, Nagra D, Dick J, Bramham K, Gordon P, Wincup C. Assessing Lupus Disease Activity Following the Onset of End-Stage Kidney Disease Within a Single Tertiary Centre in South London [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/assessing-lupus-disease-activity-following-the-onset-of-end-stage-kidney-disease-within-a-single-tertiary-centre-in-south-london/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessing-lupus-disease-activity-following-the-onset-of-end-stage-kidney-disease-within-a-single-tertiary-centre-in-south-london/