Session Information
Date: Tuesday, November 14, 2023
Title: (1945–1972) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Over the last few decades, it has been established that multiple infections can mimic idiopathic inflammatory myopathies (IIM). HIV, HTLV-1, and Lyme disease are all associated with chronic, progressive myopathies indistinguishable from IIM. While the similarities between IIM and these infectious myopathies have been reported, differences in disease course or treatment outcomes in this population with co-existing IIM and infectious myopathies has not been evaluated. Our aim was to compare the spectrum of organ involvement and treatment response in IIM patients with infections at risk for comorbid infectious myopathies in comparison to IIM patients without infections which may contribute to myositis.
Methods: A registry was created of Montefiore Medical Center patients that met 2017 EULAR/ACR classification criteria for IIM that included patient demographics, IIM subtype, clinical manifestations by organ system, comorbidities, and treatment history. Medication failure was defined by rheumatologist, discontinuation due to adverse effects, or medication change within 3 months. Medication control was defined by documented clinical improvement. Lyme and HTLV-1 statuses were based on confirmatory western blot testing and HIV status was confirmed by viral load. If these variables were positive, diagnosis date was also recorded. Statistical analysis was carried out with paired t-tests and signed rank tests. All p values < 0.05 were considered significant.
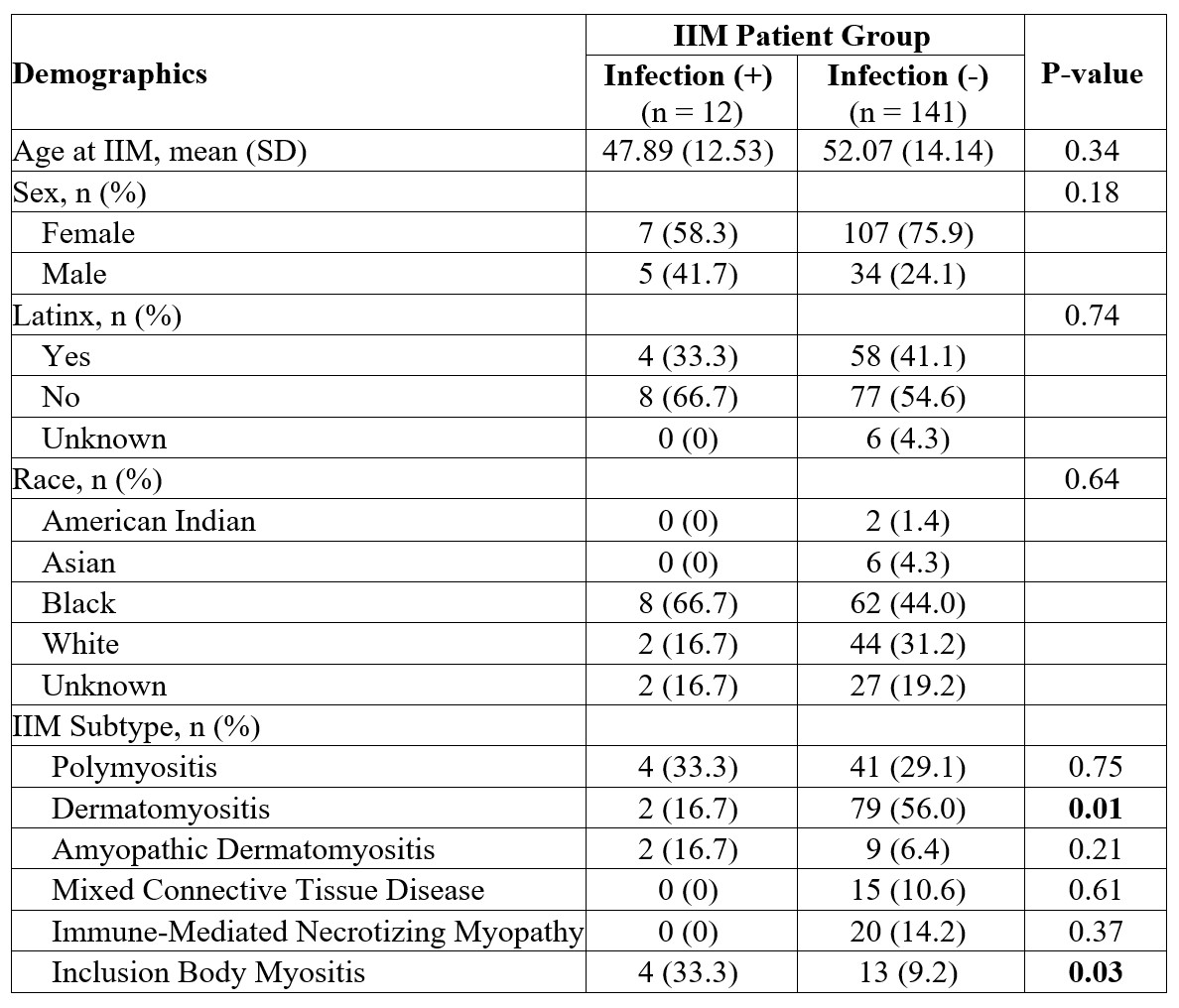
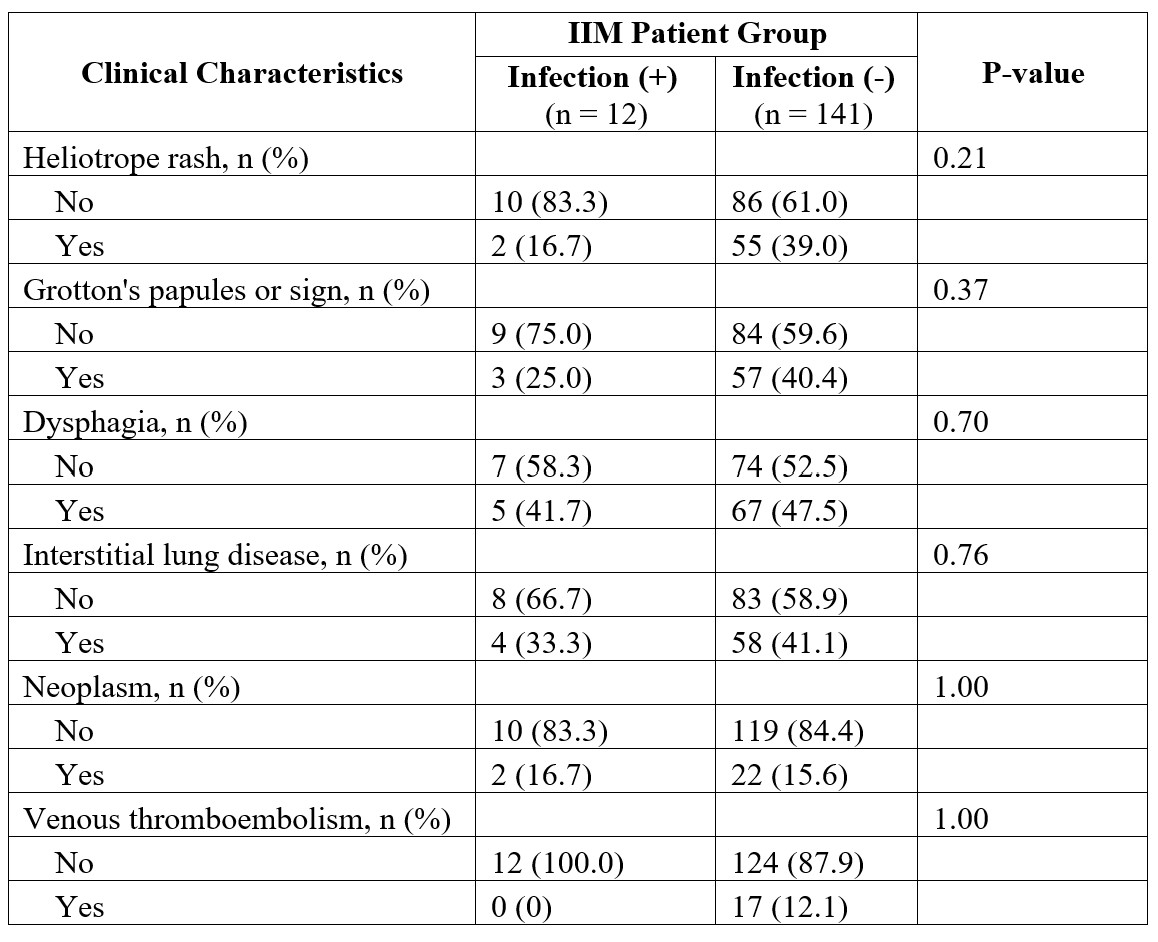
Results: Of our cohort of 153 IIM patients, 2 patients were found to have HIV, 9 were HTLV-1 positive, and one met criteria for active Lyme disease. Given the small number of patients with possible infectious myopathies, these were analyzed together in one group. Comparison of the IIM patients with infections and IIM patients without infectious comorbidities, we found a similar distribution of age, sex, Latinx ethnicity, and race between the two groups as shown in Table 1. When comparing IIM subtypes between the two groups, we found dermatomyositis was found more frequently in the non-infectious cohort (p = 0.01) and inclusion body myositis (IBM) was found more frequently in the infectious cohort (p = 0.03) (Table 1). There were no differences in cutaneous, gastrointestinal, or pulmonary manifestations between the two groups (Table 2). The rates of neoplasm and venous thrombosis complications were also comparable. There was no difference in steroid use or treatment outcomes for conventional disease-modifying agents or biologics between the two groups. In IIM patients with an infection, the infection had a median time of diagnosis 2 months prior to the IIM diagnosis.
Conclusion: While the type of IIM may be associated with infection, particularly IBM as has been reported in other literature, the presence of a infectious myopathy in IIM patients does not lead to a difference in organ involvement or treatment outcomes. The initial presentation of IIM is a crucial time for patients to be diagnosed with a concomitant infection. Further studies are needed to elucidate the link between IBM and specific infectious processes.
To cite this abstract in AMA style:
Valle A, Meisel T, Xie X, Mahmood S. Infectious Myopathies in an Urban Inflammatory Idiopathic Myopathy Cohort: Frequency and Impact on Disease Course and Treatment [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/infectious-myopathies-in-an-urban-inflammatory-idiopathic-myopathy-cohort-frequency-and-impact-on-disease-course-and-treatment/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/infectious-myopathies-in-an-urban-inflammatory-idiopathic-myopathy-cohort-frequency-and-impact-on-disease-course-and-treatment/