Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Immunosuppression for treatment of systemic autoimmune rheumatic diseases (SARDs) is associated with increased risk of severe acute COVID-19 due to blunted vaccine responses and impaired immune response to infection. Whether immunosuppression may also alter the risk for post-acute sequelae of COVID-19 (PASC), or “long COVID,” is unclear. Previous studies (Al-Aly et al, Nature Medicine, 2022) have developed electronic health record (EHR)-based definitions of PASC that have the benefit of including all COVID-19 survivors, rather than relying on prospective studies that may have selection bias, but have not been performed among SARD patients. We evaluated baseline demographic and disease factors associated with PASC in a large EHR-based cohort of patients with SARDs.
Methods: We systematically identified patients with SARDs and confirmed COVID-19 in a large healthcare system (up to 1/18/2023). We required patients to have baseline data in the EHR prior to the index date, defined as initial COVID-19 infection. Patients who survived COVID-19 were followed from 30 days after the index date until the development of any incident PASC feature, repeat COVID-19 infection, 1 year of follow-up, death, or until 4/14/2023. We evaluated the proportion with incident PASC features, defined by incident ICD codes, relevant vital signs or labs, and/or medications, extracted from the EHR. We estimated the association of baseline characteristics with the risk of PASC using multivariable Cox regression.
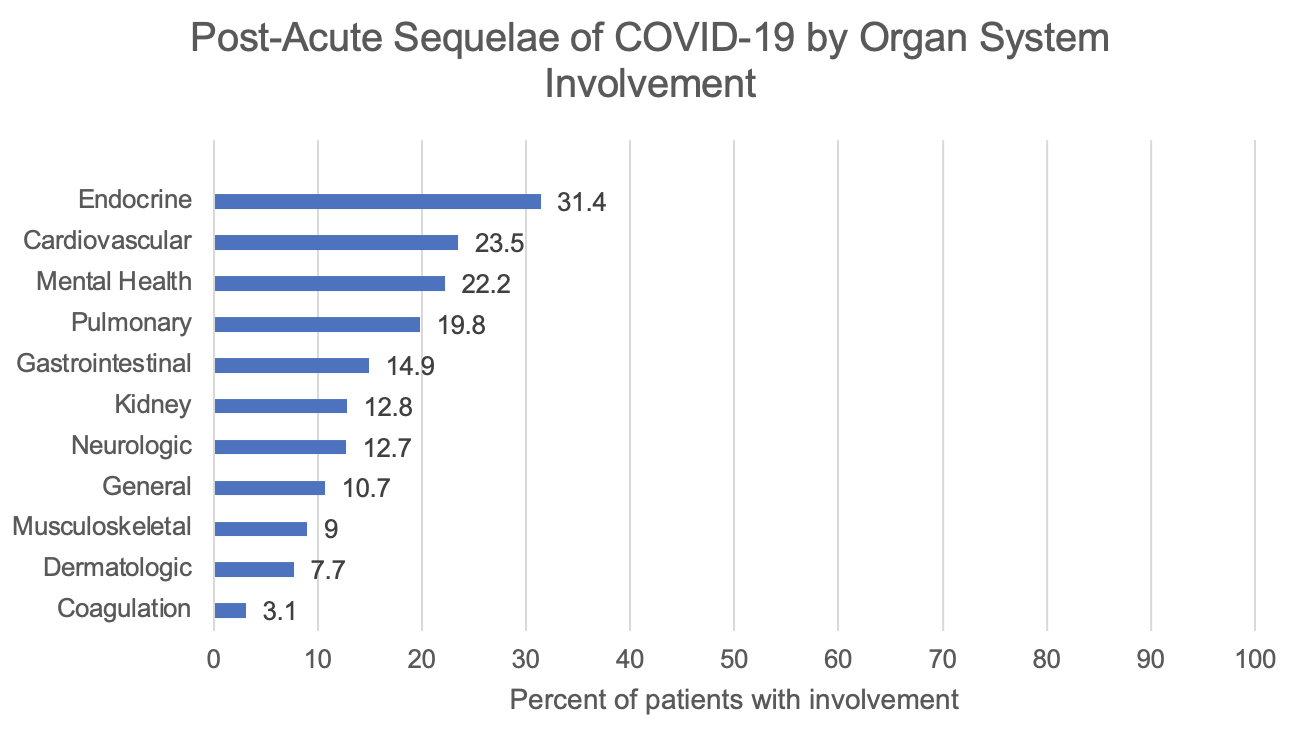
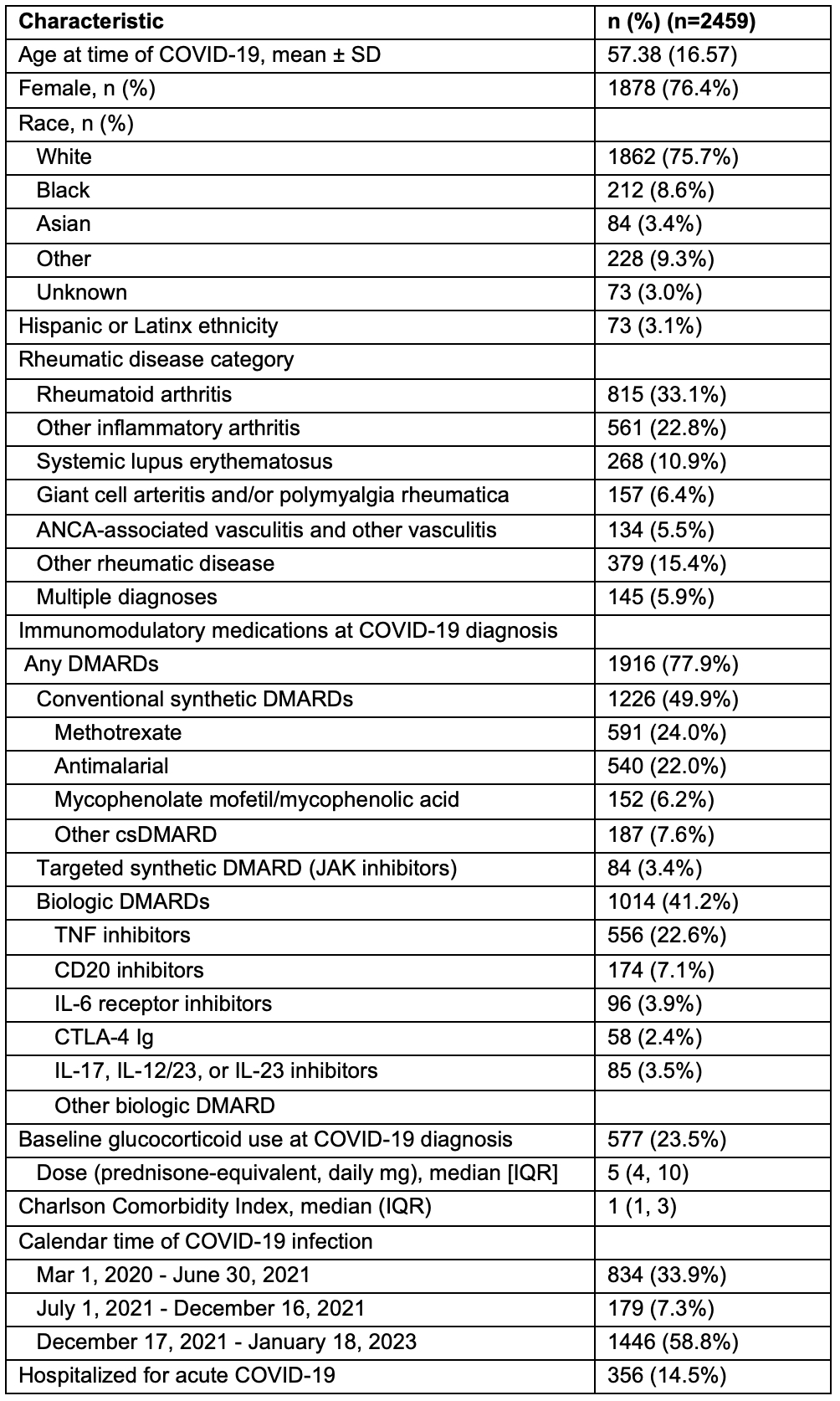
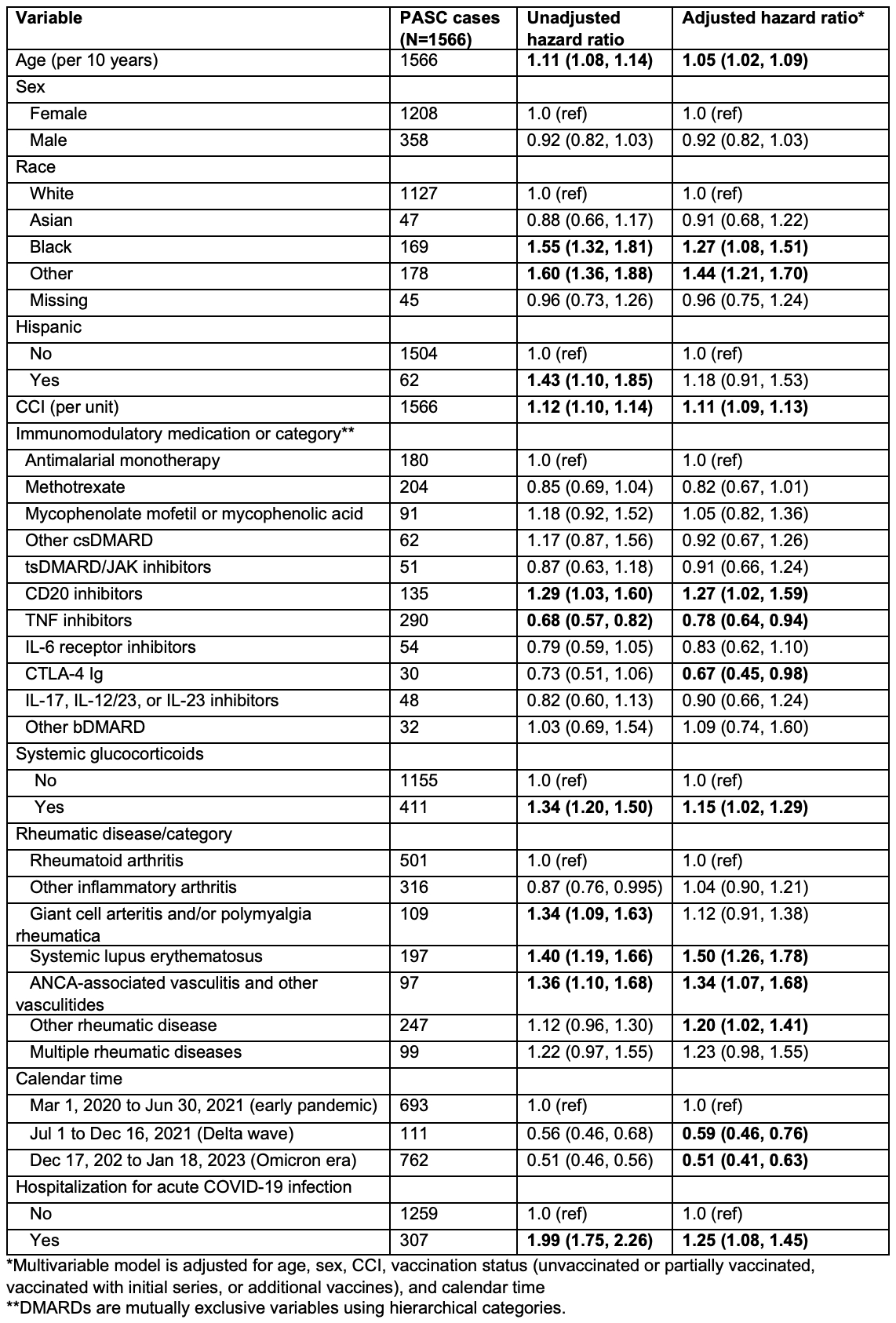
Results: We identified 2,459 patients with SARDs and confirmed COVID-19 (76% female, mean age 57 years, Table 1). The majority of patients (1566; 64%) had at least one incident feature of PASC. The most common incident PASC features were hyperlipidemia (561; 23%), anxiety (419; 17%), dyspnea (303; 12%), fatigue (263; 11%), and chest pain (246; 10%) (Figure). Compared to antimalarial monotherapy, TNF inhibitors were associated with lower PASC risk (aHR 0.78, 95% CI 0.64-0.94) and CD20 inhibitors were associated with higher PASC risk (aHR 1.27, 95% CI 1.02-1.59) (Table 2). Glucocorticoid use (vs. non-use) was associated with higher PASC risk (aHR 1.15, 95% CI 1.02-1.29). Compared to those with COVID-19 infection early in the pandemic, those with infection during the Delta wave (aHR 0.59, 95% CI 0.46-0.76) and Omicron era (aHR 0.51, 95% CI 0.41-0.63) had a lower risk of PASC. Older age, Black race, increased comorbidity burden, hospitalization for acute COVID-19 infection, and diagnosis of SLE or ANCA-associated vasculitis (compared to RA) were also associated with higher PASC risk.
Conclusion: Among patients with SARDs, CD20 inhibitor users had a higher PASC risk while TNF inhibitor users had a lower PASC risk following COVID-19 infection, suggesting that baseline immunosuppression may alter the post-acute COVID-19 course. Other factors associated with PASC included SLE or ANCA-associated vasculitis, as well as general population risk factors including calendar time (as a marker of SARS-CoV-2 variant and available treatments), older age, race, and hospitalization for acute COVID-19. These findings emphasize the potentially large burden of PASC among patients with SARDs.
To cite this abstract in AMA style:
Patel N, Wang X, Kawano Y, Schiff A, Venkat R, Cook C, Vanni K, Qian G, Bade K, Srivatsan S, Guzzo K, Williams Z, Kowalski E, Saavedra A, Sparks J, Wallace Z. Factors Associated with an Electronic Health Record-Based Definition of Post-Acute Sequelae of COVID-19 in Patients with Systemic Autoimmune Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/factors-associated-with-an-electronic-health-record-based-definition-of-post-acute-sequelae-of-covid-19-in-patients-with-systemic-autoimmune-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-an-electronic-health-record-based-definition-of-post-acute-sequelae-of-covid-19-in-patients-with-systemic-autoimmune-rheumatic-diseases/