Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: Individuals of diverse ethnic and racial backgrounds are generally underrepresented in psoriatic arthritis (PsA) research and clinical trials, despite evidence that their disease presentation, severity and course may be distinct. Here we aimed to characterize a cohort of patients with PsA to evaluate how race, ethnicity, and sex may inform features of clinical presentation, comorbidities, disease course and outcomes.
Methods: 817 consecutive patients with PsA from a large, diverse metropolitan area (NYU Psoriatic Arthritis Center, New York) were enrolled in an observational, longitudinal registry. Demographics, medical history, medication use, and psoriatic disease phenotype and activity were all recorded and analyzed.
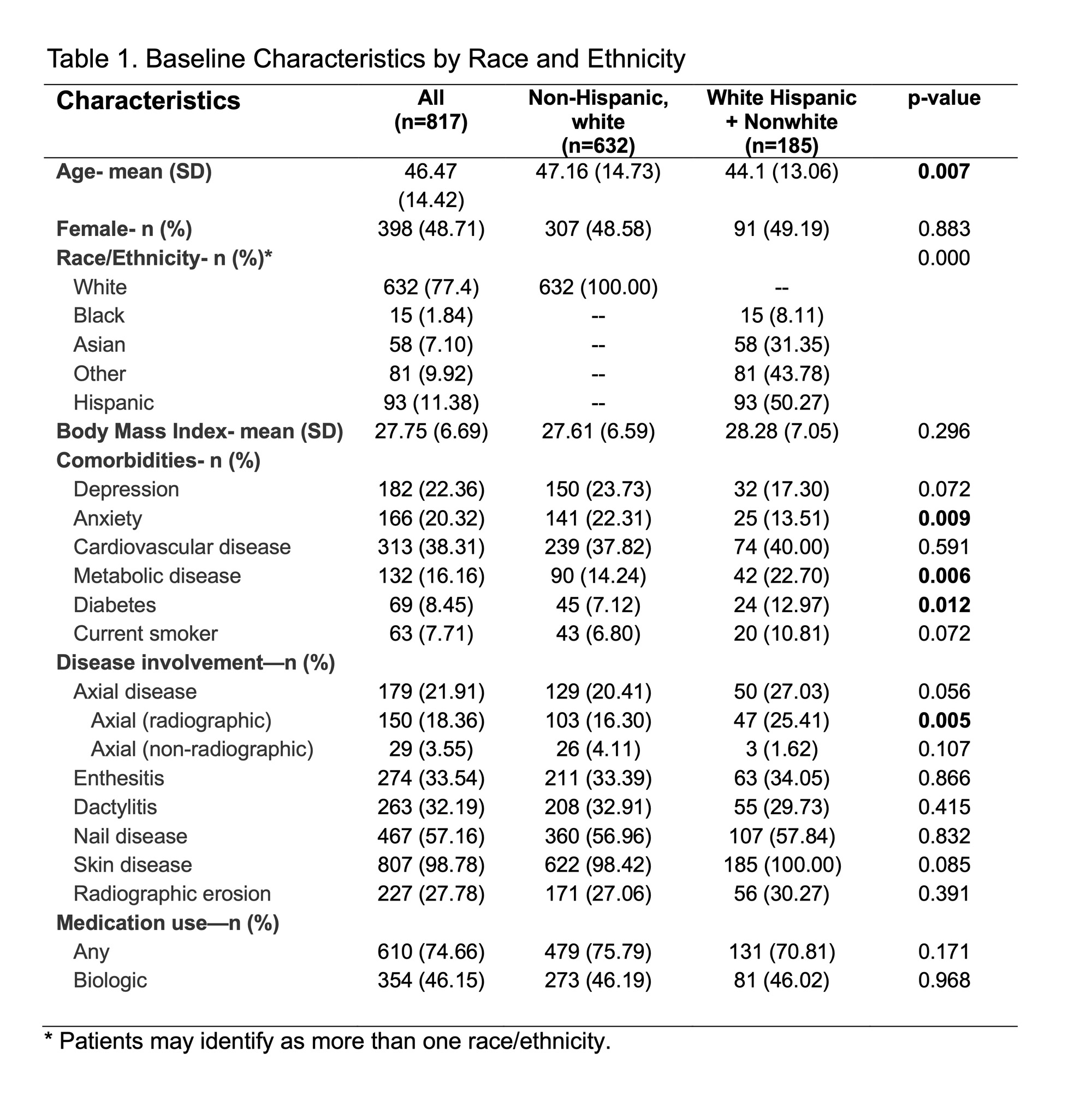
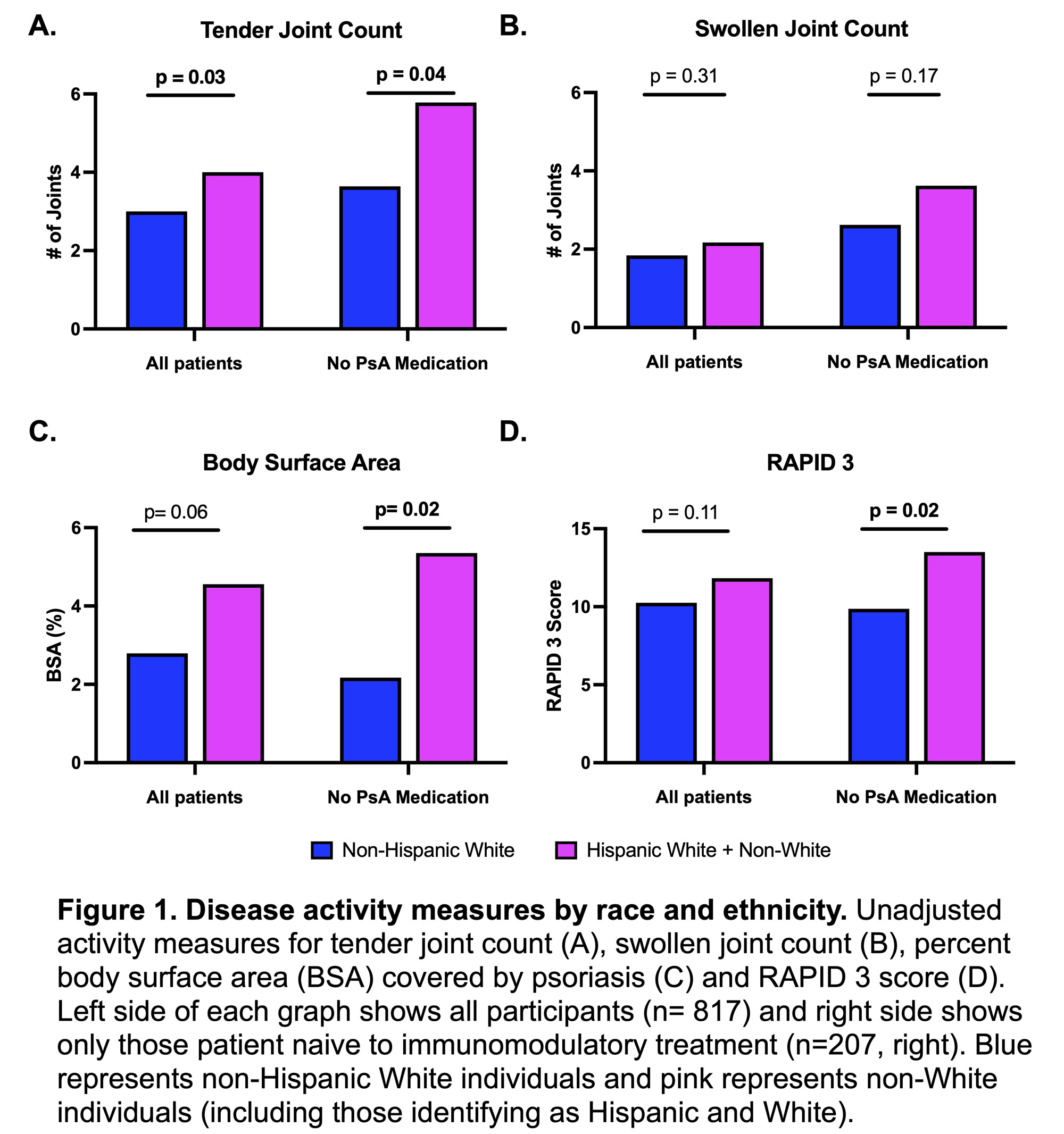
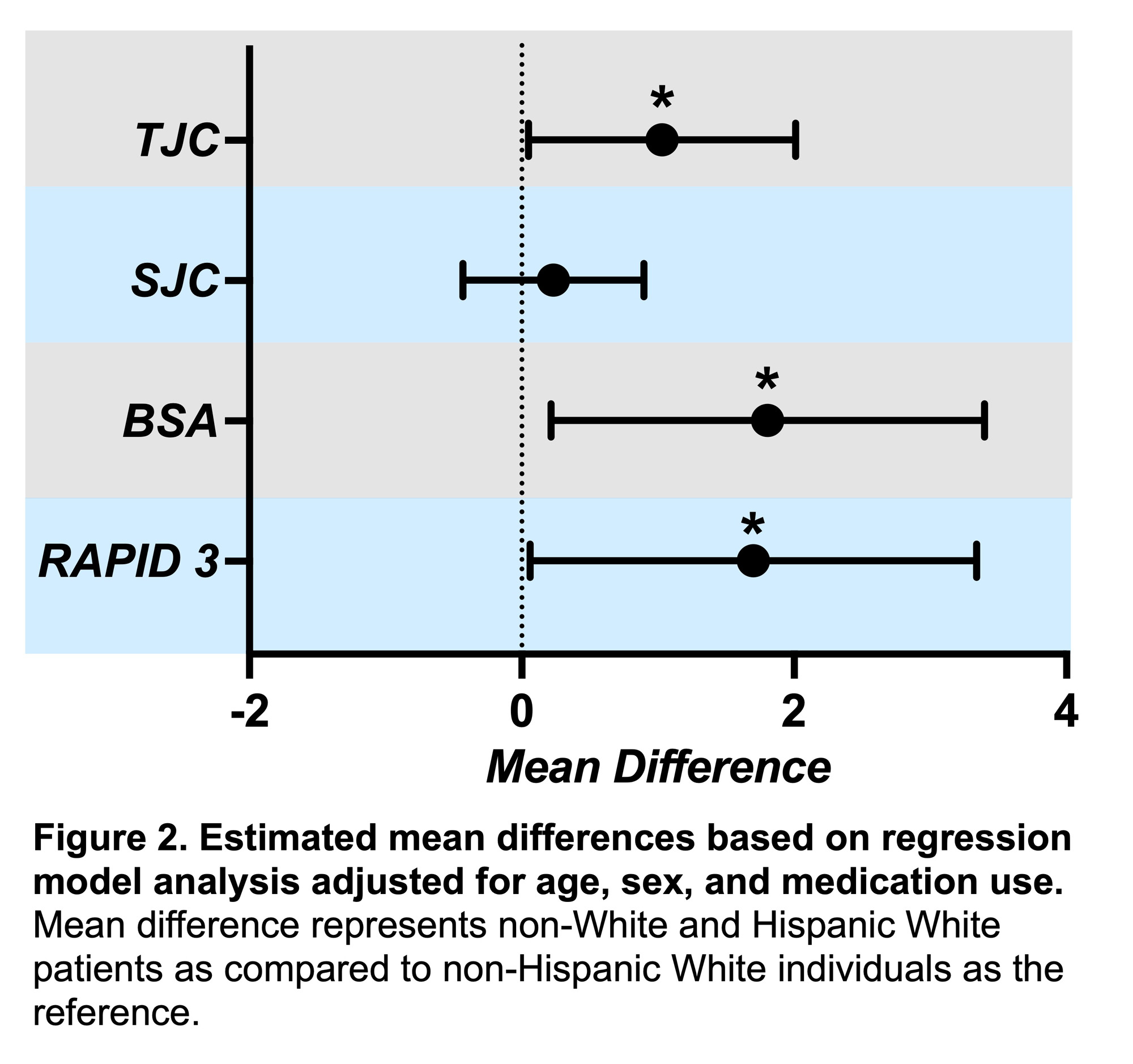
Results: The population was 77.4% non-Hispanic, White, 7.1% Asian, 1.8% Black, with 9.9% identified as other races or multiracial, and 11.8% identified as Hispanic (Table 1). Non-white individuals (include white Hispanic participants) were younger, more likely to have concomitant metabolic disease and diabetes, and less likely to have anxiety compared to non-Hispanic white individuals. Phenotypically, they were also more likely to have radiographic axial disease (p=0.005). Non-white individuals had higher tender joint counts (4.0 vs. 3.0, p=0.03) with similar swollen joint counts (2.2 vs. 1.8, p= 0.31) and proportion of individuals receiving PsA medication (70.8% vs. 75.8%, p=0.17) (Figure 1). Even when adjusting for age, sex, and medication use, the tender joint count of non-white individuals was estimated to be 1.03 joints more than white individuals (Figure 2). In the subgroup of medication naïve patients (n=207), non-white individuals also had significantly higher precent body surface area (BSA) affected by psoriasis (5.4% vs. 2.2%, p=0.02). Hispanic individuals were significantly more likely to have higher tender joint counts (4.4 vs. 3.0, p=0.03), higher RAPID3 scores (14.6 vs. 10.3, p=0.004), and moderate-severe psoriasis (30.7% vs. 17.5%, p=0.01) compared to non-Hispanic white individuals. Compared to men, women demonstrated higher RAPID3 scores (11.5 vs. 9.8, p=0.011), despite similar tender and swollen joint counts (3.5 vs. 3.0, p=0.27 and 1.8 vs. 2.0, p= 0.29 respectively) and skin involvement (3.5% BSA vs. 2.9%, p=0.37). Women continued to have higher estimated RAPID3 scores when adjusting for race/ethnicity, age, and medication use (mean difference 1.66 points higher, 95% CI 0.4-2.9, p=0.01).
Conclusion: We describe the NYU Psoriatic Arthritis Cohort, a relatively more diverse cohort compared to other registries and clinical trials, which includes 22.6% non-white individuals, mostly identifying as Asian or Hispanic. Non-white individuals had higher tender joint counts compared to white individuals despite similar swollen joint counts and medication use. Unexpectedly, they also had higher rates of radiographic axial disease. Additionally, women had higher RAPID 3 scores despite similar joint and disease measures. These findings may reflect differences in PsA presentation and outcomes as experienced by racial, ethnic, and sex groups, which need to be taken into consideration in clinical care and research design.
To cite this abstract in AMA style:
Haberman R, Ahmed T, Um S, Zhou Y, Catron S, Jano K, Moussavi S, Lydon E, Rice A, Neimann A, Reddy S, Adhikari S, Scher J. PsA Patients of Diverse Ethnic and Racial Backgrounds Experience More Skin Psoriasis, Increased Pain, and Higher Rates of Radiographic Axial Disease [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/psa-patients-of-diverse-ethnic-and-racial-backgrounds-experience-more-skin-psoriasis-increased-pain-and-higher-rates-of-radiographic-axial-disease/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/psa-patients-of-diverse-ethnic-and-racial-backgrounds-experience-more-skin-psoriasis-increased-pain-and-higher-rates-of-radiographic-axial-disease/