Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Treat-to-target is recommended in RA, but physicians often do not escalate therapy despite elevated disease activity measures due to uncertainty regarding the true degree of joint inflammation. This study evaluated the utility of ultrasound (U/S) in assessing disease activity in patients with RA with moderate disease activity measures but few swollen joints. We aimed to determine the frequency of active synovitis on U/S and compare physician treatment recommendations before and after U/S.
Methods: This single-center, prospective study enrolled adults who met 2010 ACR classification criteria for RA, had a clinical disease activity index (CDAI) >10 (moderate or high disease activity) but a swollen joint count (SJC) ≤2, and were receiving a DMARD. Patients completed surveys and underwent standardized U/S performed in the musculoskeletal (MSK) ultrasound department by a certified MSK U/S technologist using a high-resolution GE Logiq E10 system. Exams were interpreted by a single MSK U/S radiologist using the validated OMERACT scoring system, grading synovial hypertrophy by grayscale (GS) and hyperemia by power doppler (PD) in each of the bilateral MCPs, PIPs, and wrists as absent (0), minimal (1), moderate (2), or severe (3). Treating rheumatologists were surveyed pre-U/S and again after U/S to capture their impression of disease activity, confidence in their assessment (100-point scale), and treatment recommendations.
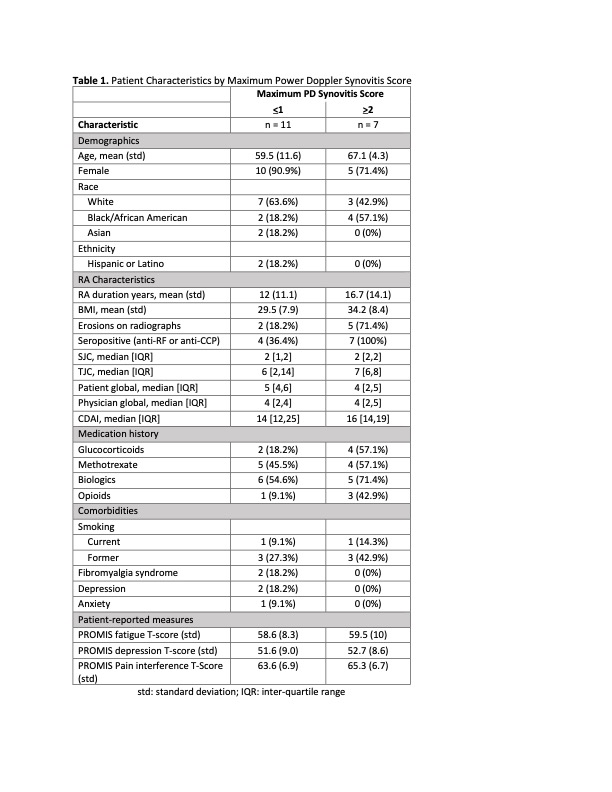
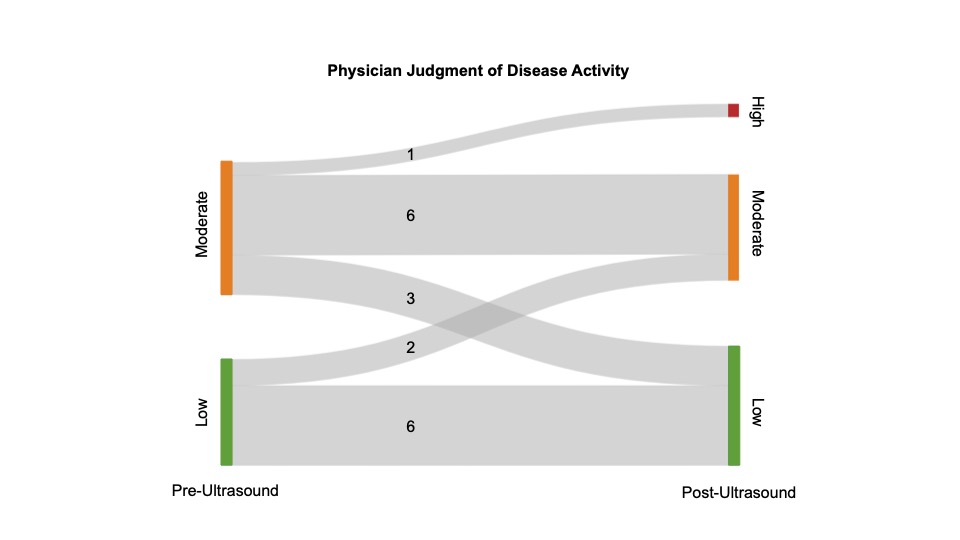
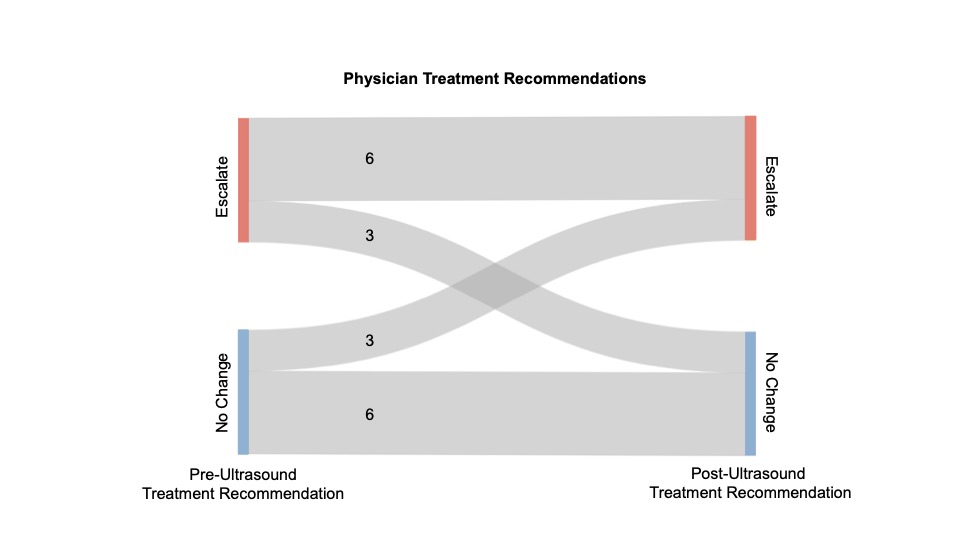
Results: We recruited 18 patients with RA: 15 (83%) females, mean age 62 years, and mean RA duration 14 years. U/S revealed moderate or severe synovial hypertrophy (GS grade 2 or 3) of at least one joint in 17/18 (94%) patients. In contrast, moderate or severe hyperemia of at least one joint (PD grade 2 or 3) was found in 7/18 (39%). Patients with active PD signal tended to be older, have longer disease duration, more frequent glucocorticoid use, higher body mass index, and more frequent seropositivity and erosions on radiographs; patient and physician global scores and PROMIS measures were similar (Table 1). Although CDAI scores indicated at least moderate disease activity pre-U/S, physician impression was that disease activity was low in 8/18 (44%) of patients pre-U/S. Physician-rated disease activity assessment changed after U/S in 6/18 (33%) patients: 3 to a higher level of disease activity and 3 to a lower level (Figure 1). Similarly, treatment decisions changed after U/S in 6/18 (33%) patients: 3 from no change to escalation of therapy and 3 from escalation to no change (Figure 1). Mean physician confidence in disease activity assessment increased from 54 pre-U/S to 72 post-U/S (p< 0.01).
Conclusion: In patients with longstanding RA, U/S demonstrating a moderate to high degree of synovial hypertrophy in at least one joint was nearly universal, but the presence of active PD signal was less common. Musculoskeletal U/S increased physician confidence in the assessment of disease activity and frequently led to a change in assessment and treatment recommendation. Future research should evaluate whether use of U/S to refine assessments of disease activity in patients with RA with high disease activity scores but few swollen joints can improve patient outcomes.
To cite this abstract in AMA style:
Song S, Kolenky O, Greenfield A, Direnzo D, Baker J, George M. Impact of Ultrasound on Physician Assessments of Patients with RA with Elevated Clinical Disease Activity Scores [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/impact-of-ultrasound-on-physician-assessments-of-patients-with-ra-with-elevated-clinical-disease-activity-scores/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-ultrasound-on-physician-assessments-of-patients-with-ra-with-elevated-clinical-disease-activity-scores/