Session Information
Date: Monday, November 13, 2023
Title: (1221–1255) Pediatric Rheumatology – Clinical Poster II: Connective Tissue Disease
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic Lupus Erythematosus (SLE) is a heterogeneous multisystemic autoimmune disorder that can cause life-threatening complications. There is a paucity of data on the utility of extracorporeal membrane oxygenation (ECMO) in children with SLE. The Extracorporeal Life Support Organization (ELSO) 2023 International summary reported an overall pediatric survival to discharge for 61% pulmonary support, 55% cardiac support, and 41% extracorporeal cardiopulmonary resuscitation (eCPR). A recent systematic analysis on the use of ECMO in children with immune-mediated disorders showed a 50% survival to discharge, including 53% pulmonary support, 55% cardiac support, and 34% eCPR. We aim to describe the use and outcomes of ECMO in childhood-onset SLE.
Methods: After approval by the ELSO Registry Committee, a retrospective cohort study from the registry database included patients < 18 years of age who had International Classification of Diseases Ninth Revision (ICD9) and Tenth Revision (ICD10) codes consistent with SLE from 2012-2022. The decision to use ECMO was made independently at each center. The primary outcome was survival to hospital discharge. Descriptive analysis on demographic information, pre-ECMO variables, ECMO mode and support indications, complications, and survival was performed using Stata v 15.1 (StataCorp, College Station, TX, USA). ECMO patient and mechanical complications were predefined by ELSO. Data on severity of illness or immunosuppression therapy was not included as it is not available in the registry.
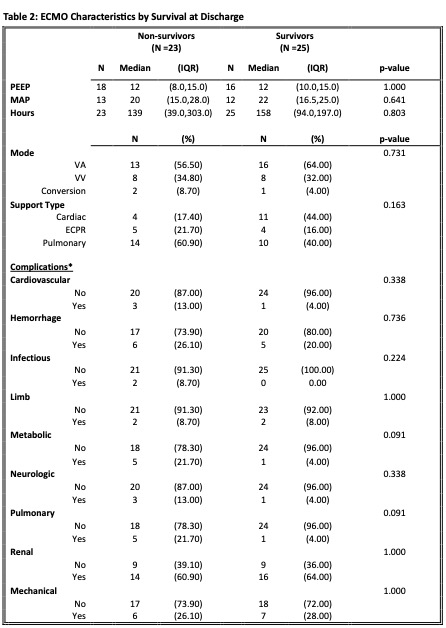
Results: During the study period, 48 children with SLE received ECMO. Table 1 show the demographics and patients comorbidities. Table 2 show ECMO characteristics for patients by survival status at discharge. Overall, 52% survived to discharge, 50% received ECMO for respiratory support (40% survival), 31% received cardiac support (44% survival), and 18% received eCPR (16% survival). The most common complications were renal dysfunction (61% non-survivors vs 64% survivors), followed by hemorrhagic (26% non-survivors vs 20%), and mechanical (26% non-survivors vs 28% survivors) complications. No ECMO parameters or patient characteristics differentiated survivors from non-survivors.
Conclusion: ECMO can be used as a life supporting therapy in children with SLE, with similar outcomes to the experience in children with immune-mediated disorders. The decision to use ECMO in this population remains challenging due to the nature of the systemic disease and potential complications related to immunosuppression. Additional analyses comparing survival rates in children and adults with lupus are underway.
To cite this abstract in AMA style:
Levin C, Ontaneda A, Guffey D, Rycus P, Anders M, Muscal E, Pereira M. Extracorporeal Life Support for Childhood-Onset Systemic Lupus Erythematosus: An ELSO Registry Analysis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/extracorporeal-life-support-for-childhood-onset-systemic-lupus-erythematosus-an-elso-registry-analysis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/extracorporeal-life-support-for-childhood-onset-systemic-lupus-erythematosus-an-elso-registry-analysis/