Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: With the rapid uptake of telehealth at the beginning of the pandemic, our group operationalized a simple strategy to convert appointments for patients who were not present at the time of their in-person visit to a telehealth visit in order to provide timely access to care amid constrained access.
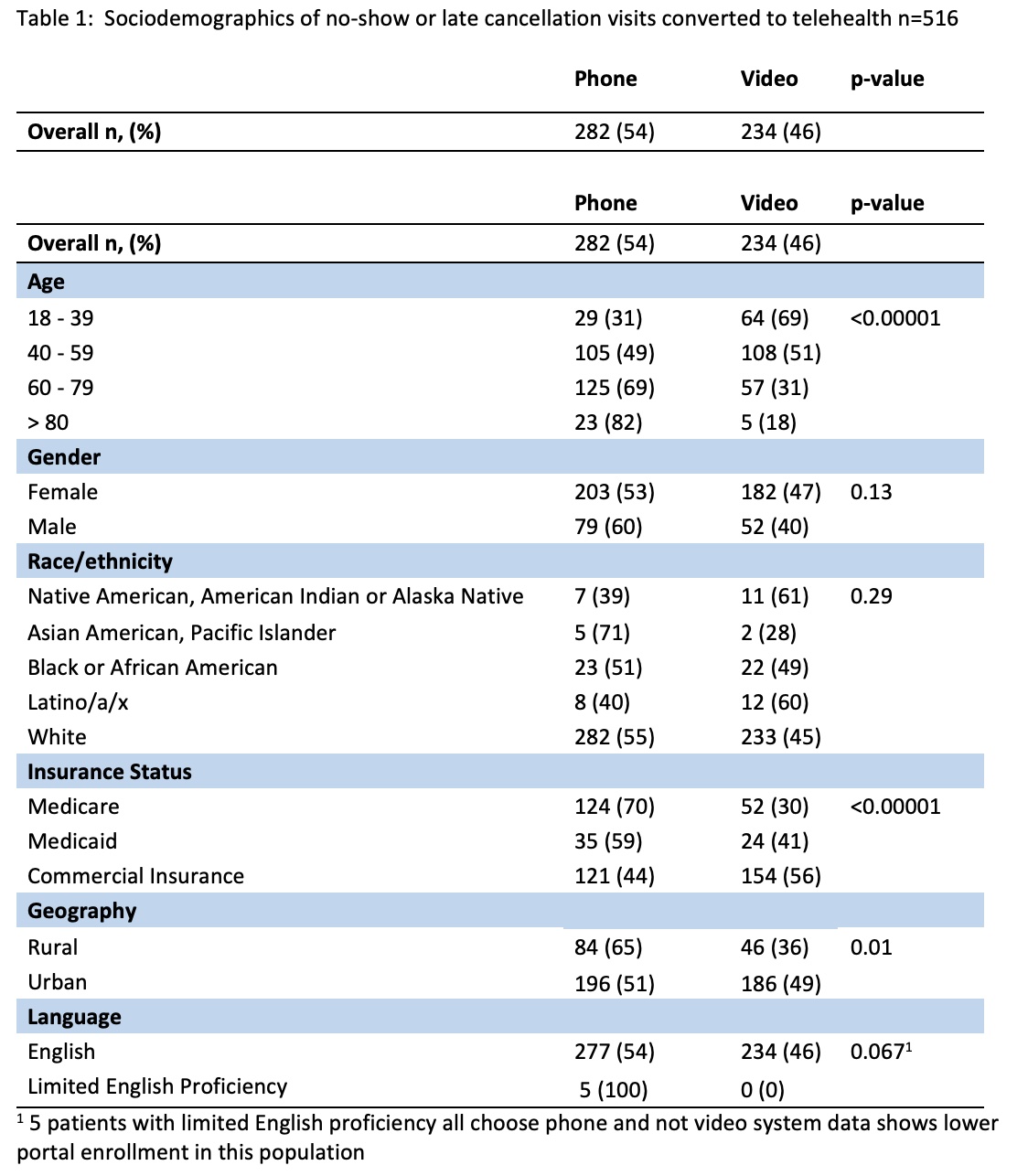
Methods: Patients with late cancellations or impending no-show visits were asked if they’d like to convert their visit to telehealth. If enrolled in the electronic patient portal a video visit was offered, and if not enrolled, a telephone visit was offered. The project was piloted at 1 clinic site through 8/31/2021 before broader implementation to 2 clinics. Procedure visits were excluded. Demographics including age, gender, race/ethnicity, insurance status, and language, were analyzed using Chi-square and Fischer’s exact tests to examine variations in telehealth visit type by group.
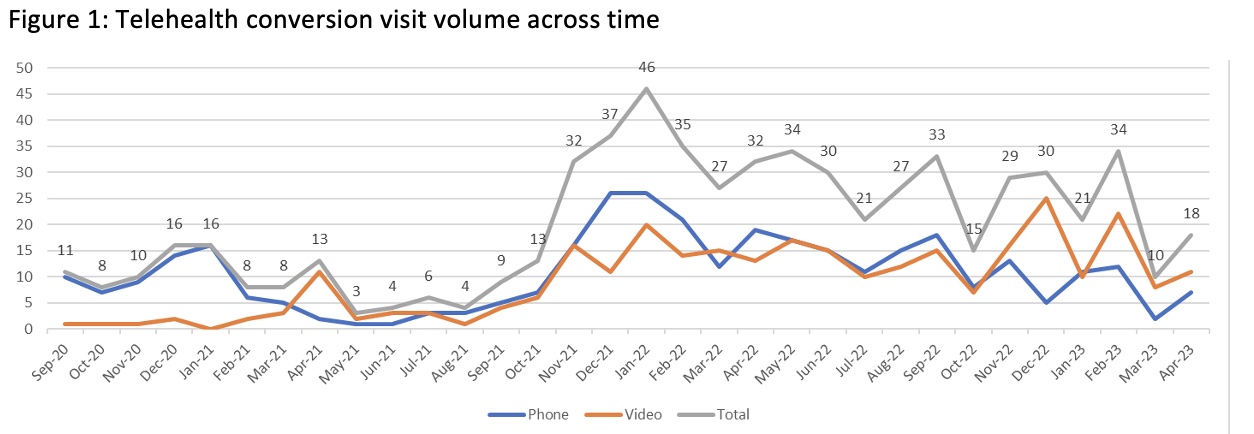
Results: Between 9/1/2023 and 3/31/2023, we successfully contacted patients across 624 visits eligible for telehealth conversion (554 unique patients) converting 83% (516/624). Of the 516 telehealth visits completed, 56% were by telephone (n= 282) and 46.2% by video (n = 234). Patients who were older or with Medicare and Medicaid public insurance were more likely to select phone visits (72.1%, 59.3%), while patients with commercial insurance were more likely to choose video visits (56%) (p < 0.001). Younger and urban patients were more likely to have video visits, while older and rural patients were more likely to have phone visits (Table 1) . There was no difference in the video vs telehealth visit selection by race, ethnicity, or sex. The intervention resulted in at least 258 additional hours of patient care, avoided reschedules and zero payment clinic time, with a modest revenue loss reduction for telemedicine of $7298 ($39.19 per appointment). Figure 1 shows overall gains and seasonal variation with higher winter demand. Monthly variability may also reflect clinic staff shortages during this period impacting outreach capacity.
Conclusion: Our simple, targeted strategy of converting appointments to telehealth when an in-person appointment is identified as at-risk resulted in significant access gains and modest revenue loss reduction. Clinic patients who are older, on Medicare or Medicaid, or rural preferred phone visits. Per literature, those with limited English proficiency are less likely to be actively enrolled in patient portals, which may impact their ability to convert to a video visit, a potential area to optimize in the future. Higher rates of telephone visits for rural patients, who may have less access to high-speed internet, highlight the equity considerations in offering telehealth modalities to patients.
To cite this abstract in AMA style:
Ferguson S, Nanes A, Zemlicka L, Bartels C. Telehealth Conversion: A Strategy for Optimizing Ambulatory Access [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/telehealth-conversion-a-strategy-for-optimizing-ambulatory-access/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/telehealth-conversion-a-strategy-for-optimizing-ambulatory-access/