Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: For end-stage inflammatory arthritis (IA) including rheumatoid arthritis (RA) and spondyloarthritis (SpA), joint arthroplasty is the only treatment option, but is considered to be a failure of medical treatment. Country-level socioeconomic factors play an important role in treatment options and long-term outcomes of IA. Though trends in arthroplasty utilization for RA and SpA have been well-studied in high-income countries, the data are still scarce in low- or middle-income countries. Understanding the trends in arthroplasty utilization in low- or intermediate-income countries would add epidemiological data on this topic and have important implications for health policy in these countries. Using the Chinese national inpatient database (i.e., the Hospital Quality Monitoring System), we aimed to examine trends in arthroplasty utilization among patients with RA, SpA, and a composite group of the IA, compared with these trends among those without IA.
Methods: Patients receiving elective primary total knee arthroplasty and total hip arthroplasty for IA or non-inflammatory conditions between 2013 and 2019 were included. The International Classification of Diseases, Tenth Revision codes were used to identify RA and SpA. Comparisons between groups were performed using the Student’s t-test for continuous variables and chi-square test for categorical variables. A generalized estimating equation model was used to examine trends over time.
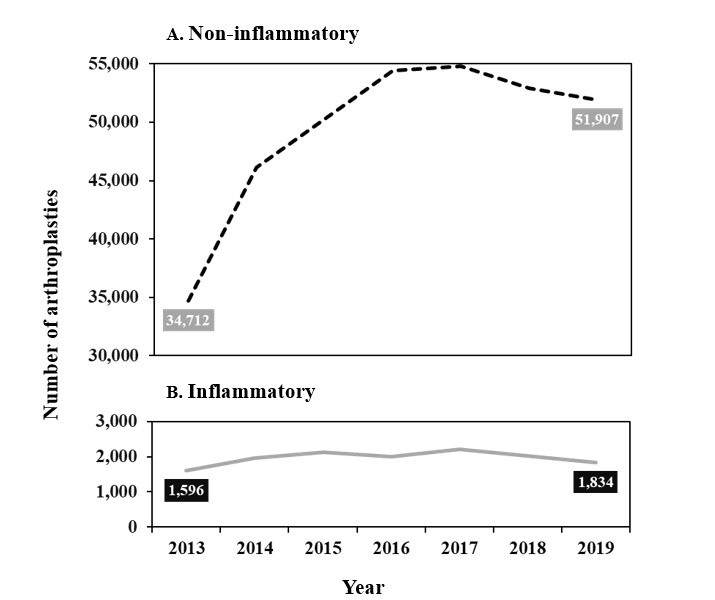
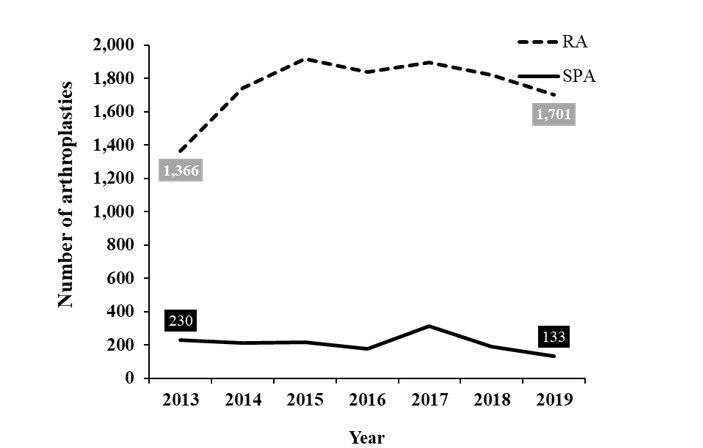
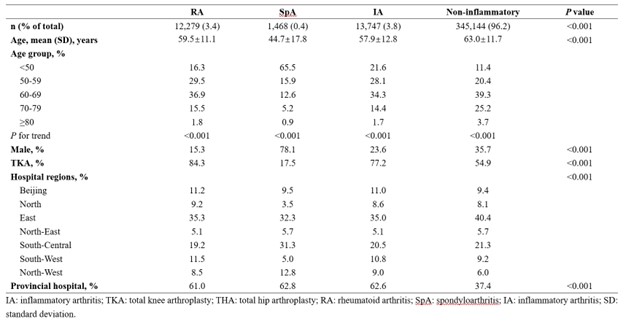
Results: Of 358,891 arthroplasties performed between 2013 and 2019, 3.8% (13,747) were performed for IA (Table 1). From 2013 to 2019, the number of arthroplasties for IA slightly increased from 1,596 to 1,834 (average yearly increase rate, 2.0%), and the number of arthroplasties for non-inflammatory conditions significantly increased from 34,712 to 51,907 (average yearly increase rate, 5.9%) (P < 0.001) (Figure 1). The proportion of arthroplasty for IA declined from 4.4% to 3.4%. In the IA group, the mean age at arthroplasty increased from 55.8 years to 59.5 years (P < 0.001), and a similar result was also found in the non-inflammatory group. The number of arthroplasties for RA increased from 1,366 to 1,701 (average yearly increase rate, 3.2%) (P < 0.001). This contrasted with the findings of SpA (average yearly decrease rate, 7.5%) (P < 0.001) (Figure 2). Age at arthroplasty increased from 58.5 years to 60.5 years in the RA group (P < 0.001) and from 39.5 years to 47.2 years in the SpA group (P < 0.001). In addition, a decrease in the proportion of arthroplasty before 50 years among RA and SpA patients was observed.
Conclusion: This nationwide inpatient-based study found that arthroplasty utilization slightly increased in RA, but significantly decreased in SpA in China. The increase in arthroplasty utilization for RA may be driven by the popularity of arthroplasty because a significant decrease in the proportion of arthroplasty for RA was observed. The decrease in arthroplasty utilization for SpA is conceivable given that economic development expanded the access to medical resource. Additionally, an increase in age at arthroplasty for RA and SpA was also found, suggesting long-term outcomes of RA and SpA are improving.
To cite this abstract in AMA style:
Xie D, Jiang Q, Wang Y, Long H, Chen H, Wei J, Li X, Wang H, Zeng C, Lei G. Trends in Arthroplasty Utilization for Inflammatory Arthritis Including Rheumatoid Arthritis and Spondyloarthritis in China: Analysis of a Large National Database [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/trends-in-arthroplasty-utilization-for-inflammatory-arthritis-including-rheumatoid-arthritis-and-spondyloarthritis-in-china-analysis-of-a-large-national-database/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trends-in-arthroplasty-utilization-for-inflammatory-arthritis-including-rheumatoid-arthritis-and-spondyloarthritis-in-china-analysis-of-a-large-national-database/