Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: Cardiovascular disease (CVD) risk is elevated in patients with SLE but underestimated by current general population prediction algorithms that do not include SLE-related variables. We aimed to develop a novel SLE-specific prediction tool, SLECRISK, to estimate CVD risk more accurately in SLE.
Methods: We studied patients in the Brigham and Women’s Hospital SLE cohort. We collected 1-year baseline data on traditional CVD risk factors, demographic and SLE-related clinical features from the electronic medical records at cohort enrollment. Ten-year follow-up for 1stmajor adverse cardiovascular event (MACE, non-fatal myocardial infarction [MI], non-fatal stroke, and cardiac death) began at day +1 after baseline period (index date). ICD-9/10 codes identified MACE, adjudicated by medical record review by board-certified cardiologists. Least absolute shrinkage and selection operator (LASSO) regression selected SLE-related variables to add to the American College of Cardiology (ACC)/American Heart Association (AHA) Pooled Cohort Risk Equations 10-year risk Cox regression model. Model fit statistics and performance for predicting moderate- and high-risk (≥10%) of MACE were assessed and compared to ACC/AHA alone, Framingham risk score (FRS), and modified FRS (FRS multiplied by 2, mFRS). Optimism adjustment was performed using bootstrapping with 300 samples.
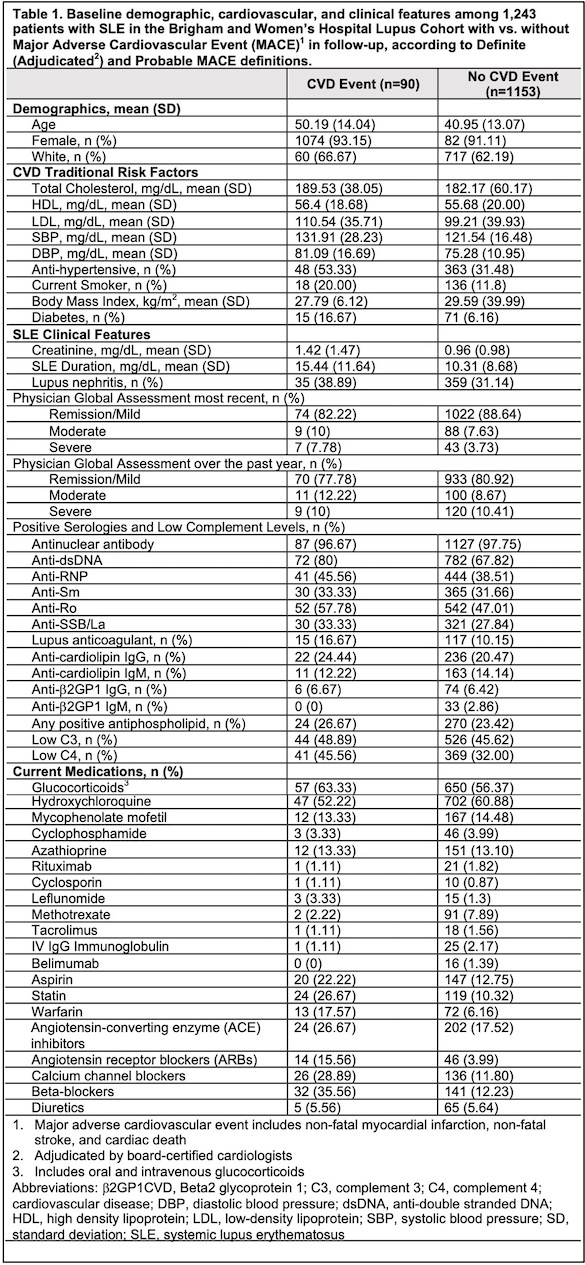
Results: We included 1,243 patients with 90 MACEs (46 MIs, 36 strokes, 19 cardiac deaths) over 8,946.5 person-years follow-up (Table 1).
Our best SLECRISK 10-Year CVD Risk equation was: 1-0.92*exp(βx-1.84), whereby βx = 5.44*Base ACC/AHA Risk Score + 0.31*disease activity (remission/mild vs. moderate/severe) + 0.04*disease duration (years) + 0.17*Creatinine (mg/dL) + 0.35*Anti-dsDNA + 0.22*Anti-RNP + 0.47*Lupus anticoagulant + 0.31*Anti-Ro + 0.49*low C4.
Sensitivity for detecting moderate/high-risk (≥10%) of MACE (0.64) and c-statistic for model discrimination (0.76) were improved vs. traditional models (Table 2). The AIC estimate of model fit improved (1190.5 to 1162.2) and Hosmer-Lemeshow goodness-of-fit tests yielded favorable results (P 0.02 in base ACC/AHA model and P 0.77 in SLECRISK), indicating good model calibration. SLECRISK identified >3-fold more high-risk patients, particularly more young women with few traditional risk factors, but more severe SLE, including lupus nephritis, higher creatinine, more autoantibodies, including antiphospholipid antibodies, hypocomplementemia, and more taking azathioprine (Fig 1).
Conclusion: We derived and internally validated a novel SLE-specific CVD risk tool based on the ACC/AHA score and SLE-related factors. SLECRISK was more sensitive and accurate than the traditional CVD generic tools for predicting moderate- and high-risk for MACE over 10 years of follow-up. If externally validated, SLECRISK may be incorporated into SLE management guidelines to help guide decision-making in the primary prevention of CVD in clinical practice.
To cite this abstract in AMA style:
Choi M, Guan H, Yoshida K, Kargere B, Ellrodt J, Stevens E, Cai T, Everett B, Weber B, Costenbader K. Personalizing Cardiovascular Risk Prediction for Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/personalizing-cardiovascular-risk-prediction-for-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/personalizing-cardiovascular-risk-prediction-for-patients-with-systemic-lupus-erythematosus/