Session Information
Date: Sunday, November 12, 2023
Title: (0691–0721) Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Atrial fibrillation is the most commonly treated cardiac arrhythmia, associated with significant morbidity and mortality. Recent research is suggestive that autoimmunity and inflammation might have a role in the pathophysiology of atrial fibrillation (AF). While several autoimmune conditions are associated with AF, autoimmune vasculitis confers a worse survival in patients with AF. Current literature is limited in determining the impact of large vessel vasculitis (LVV) in AF patients. We present a study discussing the cardiovascular outcomes in patients with LVV and atrial fibrillation.
Methods: We queried the National Inpatient Sample database in the period between 2016 – 2019. Primary AF hospitalizations were identified and subsequently we stratified the cohort based on the presence of LVV. The adjusted odds ratios (aOR) of in-hospital outcomes and resource utilization were calculated using chi-square statistics in software STATA v.17.
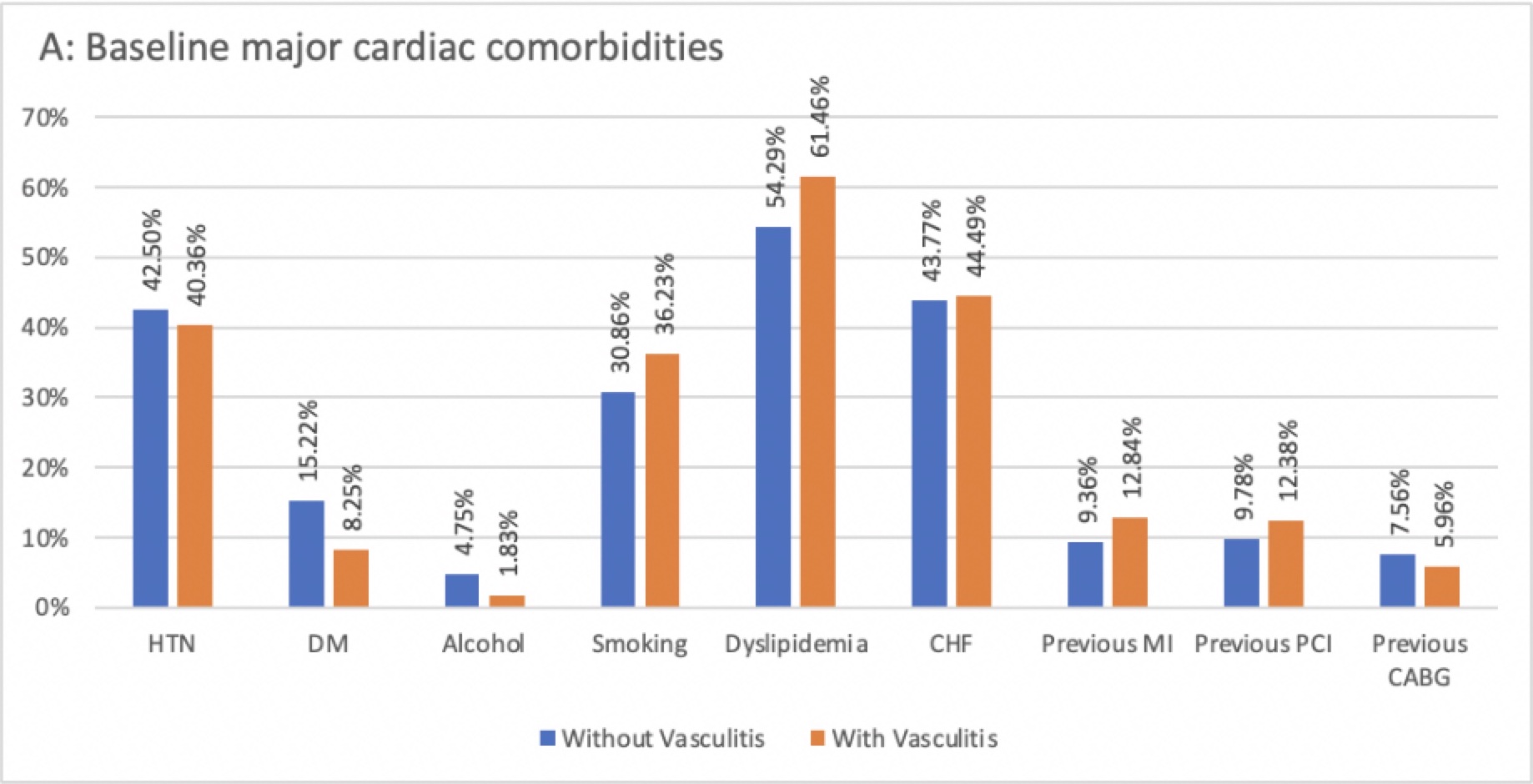
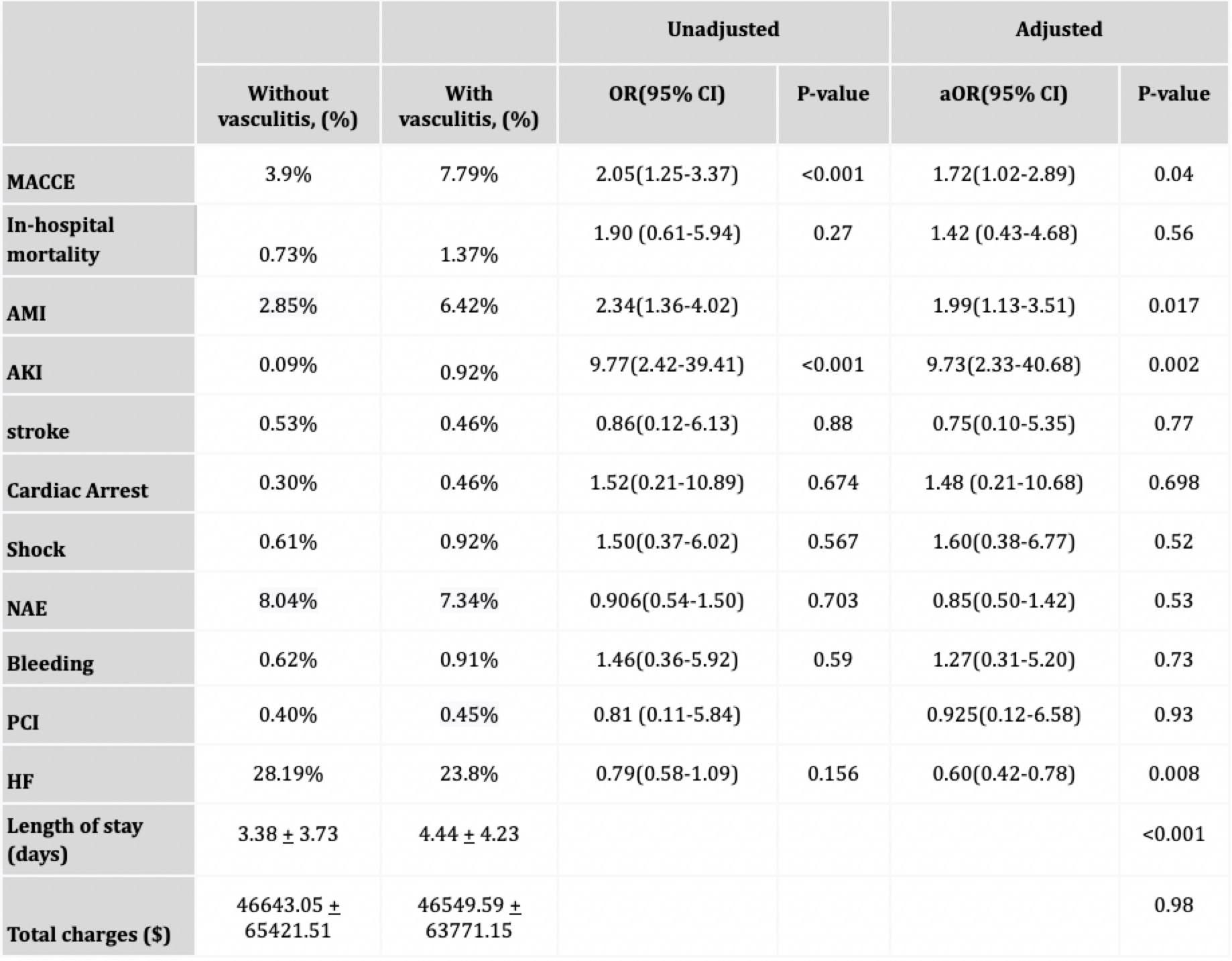
Results: Of 1,041,670 AF hospitalizations between 2016-2019; 1,090 had LVV (Giant cell arteritis: 1050 and Takayasu arteritis: 40). Afib with LVV patients were older (78.33 vs. 71.04, p< 0.001) and predominantly female (71.55 vs. 51.39, p< 0.001). On adjusted analysis, compared to non-LVV patients, LVV patients had significantly higher MACCE (aOR 1.72, 95% CI 1.02-2.89), AMI (aOR 1.99, 95% CI 1.13-3.51), AKI (aOR 9.73, 95% CI 2.33-40.68) with longer length of stay (3.38±3.73 vs. 4.44±4.23). Interestingly, there seemed to be a reduced risk of heart failure in AF patients with vs without vasculitis (aOR 0.60, 95% CI 0.42-0.78). On the contrary, there was no difference in in-hospital mortality, stroke, bleeding, need for PCI and total charge of hospitalization between the two groups.
Conclusion: The clinical outcomes in patients with concurrent LVV and AF are significantly worse, as evidenced by increased risk of MACCE, AMI and AKI compared to patients with only AF but not LVV. This study provides evidence that patients with large vessel vasculitis and AF need to be managed more aggressively as clinical outcomes are notably worse. However, we do not have enough data to suggest whether patients with LVV need to be screened for AF. Further prospective trials are needed to answer these queries.
To cite this abstract in AMA style:
Usmani S, Raksadawan Y, Taha A, Sandhyavenu H, Patel J, Goni T, Waqar Younas H, Badu I. Impact and Cardiovascular Outcomes of Large Vessel Vasculitis in Atrial Fibrillation Hospitalization: A Nationwide Inpatient Database Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/impact-and-cardiovascular-outcomes-of-large-vessel-vasculitis-in-atrial-fibrillation-hospitalization-a-nationwide-inpatient-database-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-and-cardiovascular-outcomes-of-large-vessel-vasculitis-in-atrial-fibrillation-hospitalization-a-nationwide-inpatient-database-study/