Session Information
Date: Sunday, November 12, 2023
Title: (0176–0195) Healthcare Disparities in Rheumatology Poster I: Lupus
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Cardiovascular disease (CVD) is a major cause of mortality among patients with systemic autoimmune disease. Patients with systemic lupus erythematosus (SLE) exhibit accelerated cardiovascular disease compared with age matched healthy controls. While Black and Latino patients with SLE have worse autoimmune disease than white patients, understanding of SLE-associated CVD in these marginalized patients has been limited by the exclusion of Black and Latino patients from these studies. We aim to assess cardiovascular risk in Black and Latino patients with SLE.
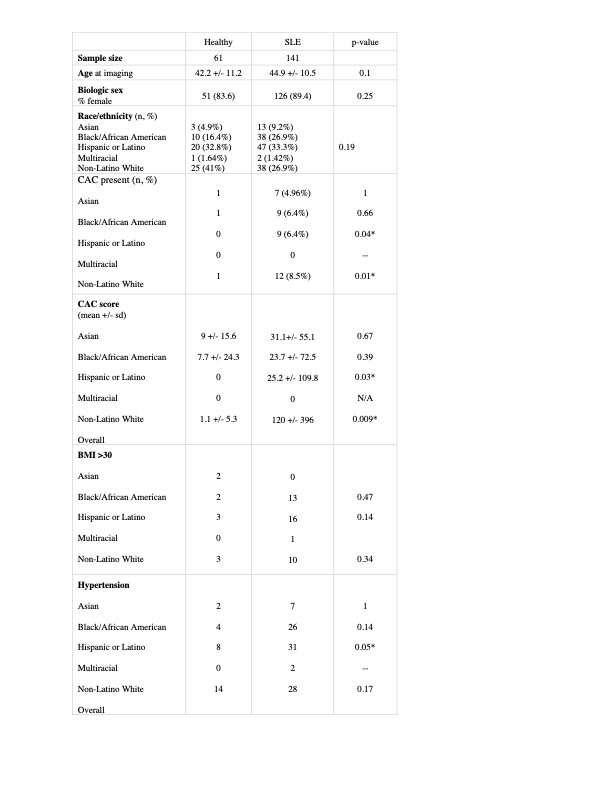
Methods: Retrospective cohort study of patients enrolled in a single center SLE natural history study. Healthy volunteers and patients with SLEwho had cardiac CT imaging from 2003-2023 were selected for review. Variables of interest were obtained at the time of imaging, and include coronary artery calcium score (CAC), patient demographics, statin use, Framingham CVD risk factors, and laboratory parameters (total cholesterol, HDL). Data were analyzed by Wilcoxon rank sum test or Fisher’s exact test when appropriate, and a p-value < 0.05 was considered statistically significant.
Results: There were 61 healthy and 141 SLE patients available for review. Of the patients with SLE, 89% were women and the average age at the time of imaging was 45 years. 27% identified as Black/African American and 33% identified as Hispanic Latino. CAC was present in 26% of the SLE patients with a mean CAC score of 49.9, while in healthy controls, CAC was present in 5% of volunteers with a mean CAC score of 2.6. Hypertension was present in 47.5% of healthy controls and 68% of SLE patients (p=0.007). Comparison of other CVD risk factors including obesity, any smoking history, cholesterol level, and diabetes mellitus did not reveal any significant differences between groups. Mean HDL was 58.5 in SLE patients without significant differences between groups. Use of statin in SLE patients with an elevated CAC score was 16%.
Conclusion: Our preliminary findings describe a multi-ethnic cohort of patients with SLE. CAC was present in 26% of affected patients and 5% of healthy controls. CAC was more prevalent and higher in white patients compared to Black and Latino patients. While hypertension was more prevalent patients with SLE, many other traditional risk factors were not present. We found that Black and Latino patients with SLE had significantly lower mean CAC scores when compared to non-Latino white patients. Our findings may indicate that calcium scores are not as reliable of a risk factor to guide secondary prevention in Black and Latino patients with SLE. It may be that Black and Latino patients have more non-calcified plaque burden when compared to non-Latino white patients with SLE. Further study is needed to examine mechanisms to explain these differences and replicate our findings in larger groups. These findings begin to address CVD health disparities in marginalized populations by providing additional information on SLE-associated CVD in Black and Latino patient
To cite this abstract in AMA style:
Gonzalez G, Manna Z, Fike A, Chu J, Hasni s, Dizon B. Assessing Cardiovascular Risk in Black and Latino Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/assessing-cardiovascular-risk-in-black-and-latino-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessing-cardiovascular-risk-in-black-and-latino-patients-with-systemic-lupus-erythematosus/