Session Information
Session Type: Poster Session B
Session Time: 5:00PM-6:00PM
Background/Purpose: Children with childhood-onset systemic lupus erythematosus (cSLE) experience more severe disease than their adult counterparts, in addition to high rates of clinical depressive symptoms (30%) and fatigue (65%) (1). A “high- risk” profile categorized by clinically elevated depressive symptoms and fatigue has been shown to be related to reduced health-related quality of life and poorer patient outcomes in cSLE patients (2). The Treatment and Education Approach for CHildhood-onset lupus (TEACH) is a tailored cognitive behavioral therapy (CBT) for youth with cSLE that may address these symptoms. (3). TEACH is currently being tested in an RCT with promising results after 6 weeks. However, it is unknown how the “high- risk” group may respond to this program. This study aims to assess the impact of risk status on the outcomes of cSLE patients undergoing CBT.
Methods: This study uses data from an ongoing multisite clinical trial of youth (average age of 17 years, 100% female, 70% identifying as from a minority group, n=46/60 currently completed evaluation for the study). All of these patients met the ACR criteria for cSLE. 16 of these youth have thus far been randomized to and completed TEACH. They were grouped into low- or high-risk categories based on baseline depression and fatigue t-scores ( >70; >2SD from mean) (3). Repeated measures ANOVAs were conducted to compare the low- and high-risk groups pre and post 6 week TEACH protocol for main study outcomes (e.g. depressive symptoms (CDI-II), fatigue (PROMIS), and pain (VAS)) and additional exploratory outcomes (anxiety (SCARED), disease severity (SLEDAI), and health-related quality of life (Peds-QL)). Independent samples t-test was used to determine if baseline outcome measures were significantly different between low- and high-risk groups.
Results: Out of the 16 patients who have completed the TEACH protocol, 6 (37.5%) met criteria for inclusion in the high-risk group. There was no significant difference between risk groups based on age, disease duration, or self-reported race. There was a significant difference between groups in baseline depression scores only (p= 0.005). At week 6 after completion of TEACH, depression scores decreased by 26% in the high- risk group, while the low- risk group only decreased 6% (p< 0.001; Table 1). Fatigue, anxiety, health-related quality of life, and disease severity followed the same trends (see Figure 1). Despite these trends, there were no significant differences found between the low- and high-risk groups in any outcomes other than depressive symptoms.
Conclusion: There is very little literature on nonpharmacologic treatments for cSLE like CBT (4). These data reveal interesting trends that CBT may be more effective in cSLE patients with high levels of fatigue and depression. Some results may be driven by the fact that the high-risk group begins with higher baseline symptoms. Lack of significant difference between groups may be attributed to a small sample size and these analyses should be replicated with a larger data set (e.g., upon completion of the RCT) in the future. Although the high-risk group shows more improvement overall, this should not shadow that both high- and low- risk groups had improved outcomes with the TEACH protocol.
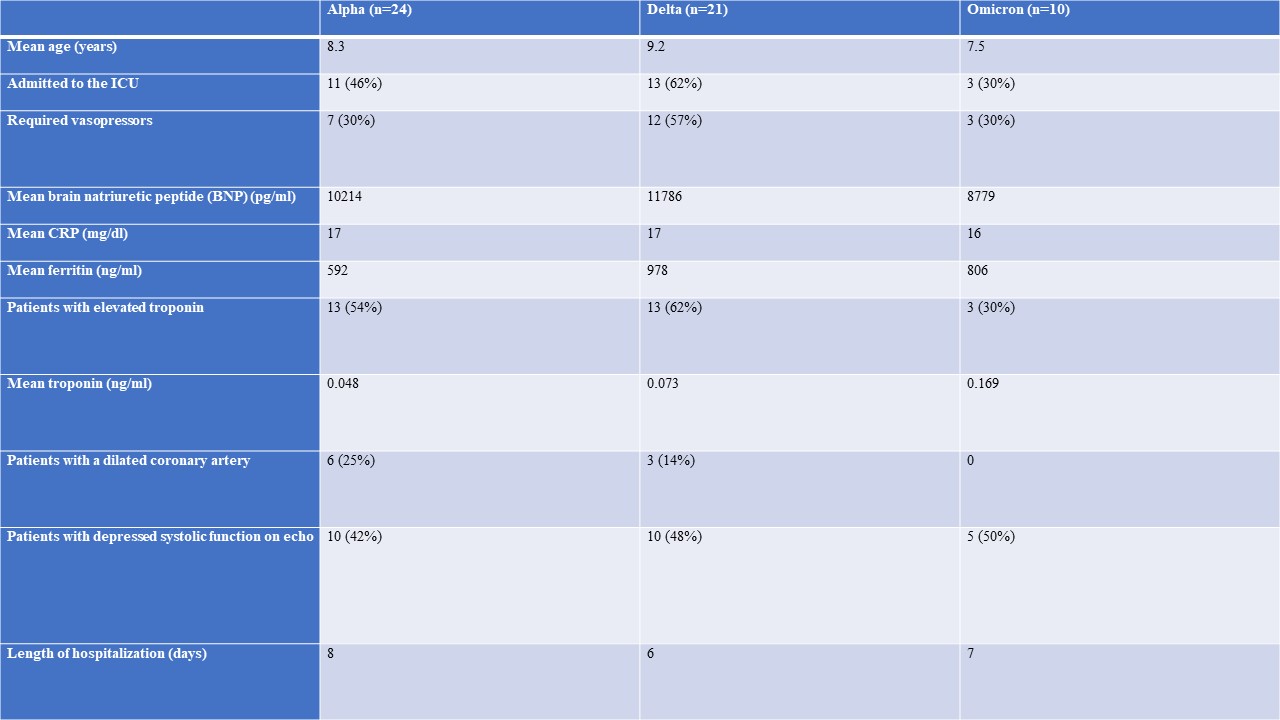 Comparison of MIS-C between the COVID variants. Emergence of dominant variants was defined by the CDC’s infection rates.
Comparison of MIS-C between the COVID variants. Emergence of dominant variants was defined by the CDC’s infection rates.
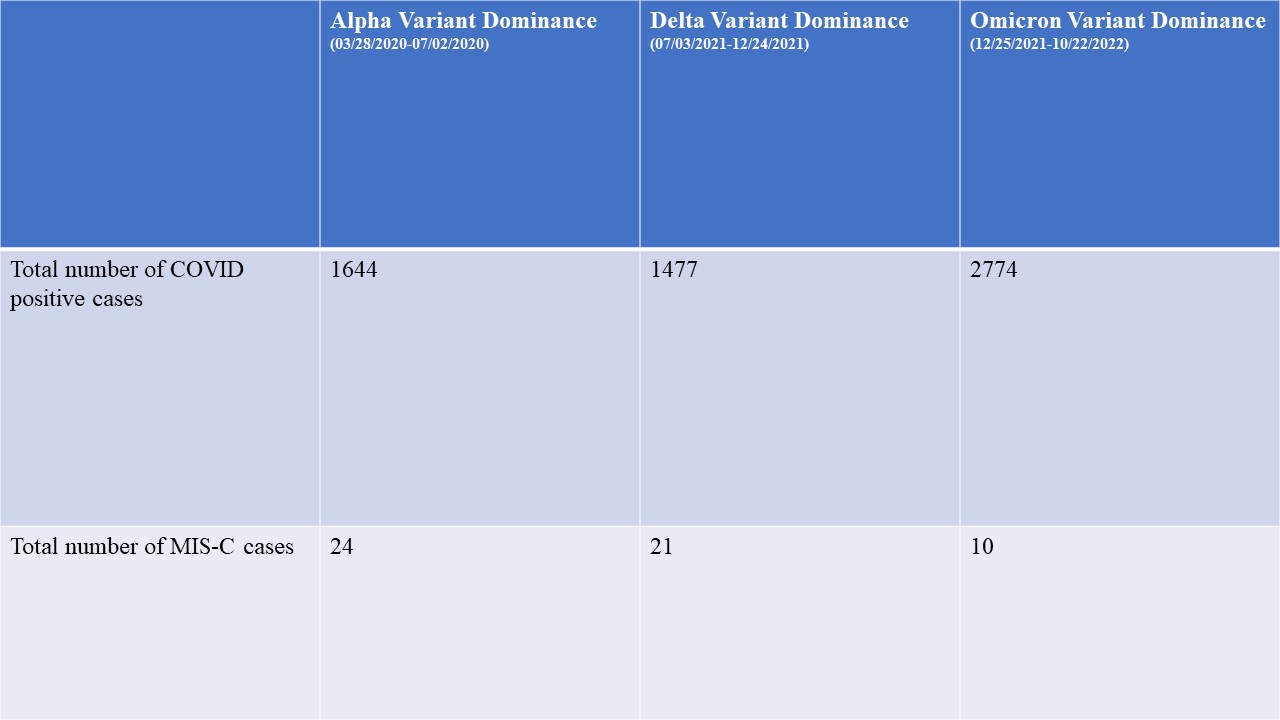 COVID and MIS-C incidence rates for each COVID variant.
COVID and MIS-C incidence rates for each COVID variant.
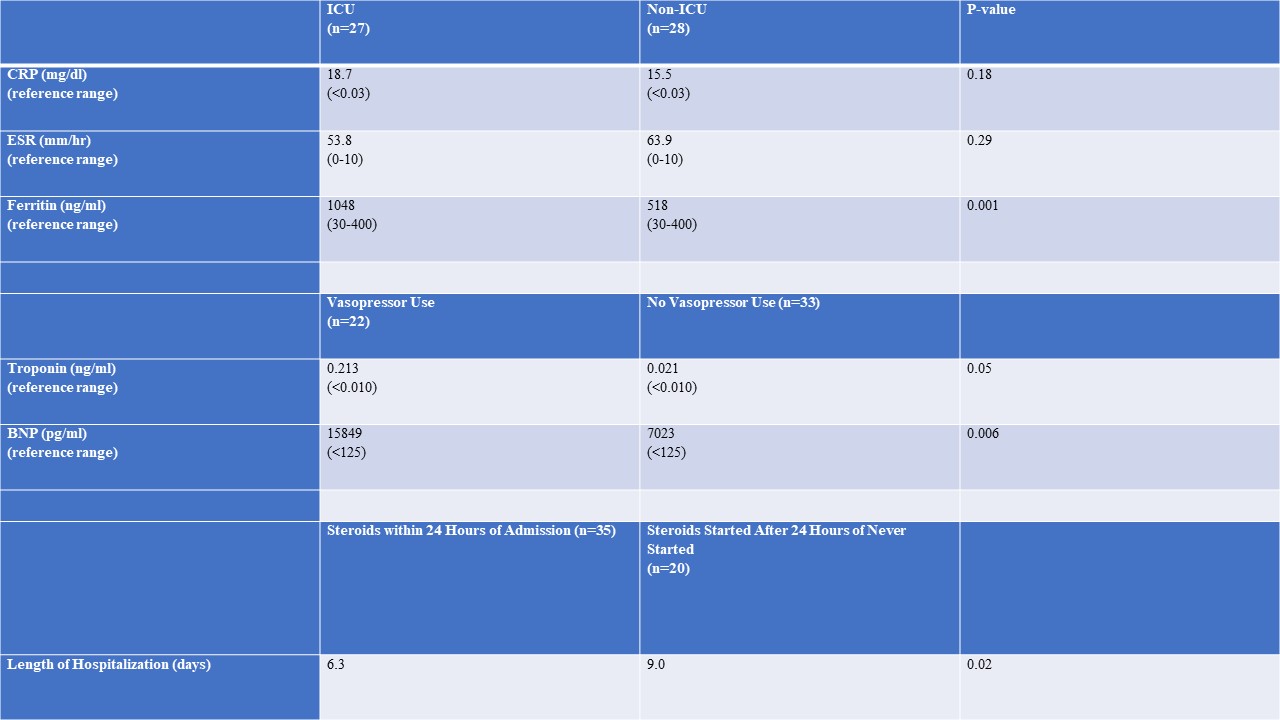 Comparison of mean laboratory values and length of hospitalization for all patients with MIS-C. Mean CRP, ESR, and Ferritin values are compared between patients admitted and not admitted to the ICU. Cardiac markers (troponin and BNP) are compared between patients who required vasopressors and patients who did not. Length of hospitalization is compared between patients who received steroids within 24 hours of admission and those who received steroids later or not at all.
Comparison of mean laboratory values and length of hospitalization for all patients with MIS-C. Mean CRP, ESR, and Ferritin values are compared between patients admitted and not admitted to the ICU. Cardiac markers (troponin and BNP) are compared between patients who required vasopressors and patients who did not. Length of hospitalization is compared between patients who received steroids within 24 hours of admission and those who received steroids later or not at all.
To cite this abstract in AMA style:
Begezda A. A Descriptive Study of Patients with Multisystem Inflammatory Syndrome in Children [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/a-descriptive-study-of-patients-with-multisystem-inflammatory-syndrome-in-children/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-descriptive-study-of-patients-with-multisystem-inflammatory-syndrome-in-children/
