Session Information
Session Type: Poster Session B
Session Time: 5:00PM-6:00PM
Background/Purpose: Pediatric Rhupus syndrome is a complex autoimmune disease characterized by overlapping clinical and immunological features of Juvenile Idiopathic Arthritis (JIA) and juvenile Systemic Lupus Erythematosus (jSLE). Pediatric presentation of Rhupus is rare. The need for established clinical and serological diagnostic criteria and the low incidence rate make Rhupus identification difficult. Through a systematic literature review, we aim to exhibit common clinical and serological characteristics in children presenting this disease.
Methods:We performed a systematic literature review of clinical features of pediatric Rhupus syndrome through Pubmed, Scopus, EBSCO, and Google Scholar following PRISMA guidelines (Figure 1). Our search terms included:((Rhupus) AND (pediatric OR pediatrics OR children OR adolescence OR paediatric OR paediatrics OR child)). Inclusion criteria were: population with an initial manifestation of JIA with simultaneous or subsequent onset of Rhupus syndrome with an age less than 18 years old. Only cross-sectional, retrospective and prospective cohort studies, case reports, and case series studies published between 2000 and 2023 were considered.
Results:Among 564 articles collected using Pubmed, Scopus, Google Scholar, and the EBSCO database, only 13 articles met the inclusion criteria. Just 8 case reports and 5 case series with 26 patients of whom the clinical manifestations, serologic, and imaging findings in pediatric Rhupus patients were recorded. The mean age of patients with Rhupus syndrome was 11 years old, 80% of females and 19% of males (Figure 2). Overall, the first manifestation was articular involvement with the predisposition of erosive patterns, including big articulations. Erosive arthritis was presented in 73% of patients, followed by juxta-articular osteopenia in 21%, chronic synovitis in 15%, joint space narrowing in 10%, and 5% of patients presenting synovial thickening, effusions, and no joint erosions. Ankle arthritis was reported in 65% of patients, followed by arthritis of knees in 50%, wrists in 25%, PIP in 10%, DIP in 10%, and hip involvement in 5%. Of the 26 patients reported, 69% had Rheumatoid factor +, 26% were anti-CCP+, 73% had ANA+, 46% had ds-DNA positive, 19% were anti-Smith+, and 11% were antiphospholipid positive. After being diagnosed with Rhupus Syndrome, a systemic involvement was presented in most patients: 64% had renal involvement, 11% exhibited neurological complications, 11% presented hematologic manifestations, 17% had other sequels, and 23% reported no disease complications. These findings are presented in Table 1.
Conclusion:This comprehensive review invites physicians to consider Rhupus Syndrome in patients with erosive arthritis that is unusually seen in jSLE. Despite our extensive systematic review, only a few cases were found which suggests the underreport or underdiagnosis of these cases. We invite more specialists to report the nature of this illness to reach a consensus on diagnosis and management for preventing delayed sequels of this pathology. Close follow-up with extensive clinical, serological, and imaging studies is essential to improve these patients’ medical care and quality of life, especially in the setting of erosive arthritis in patients with lupus.
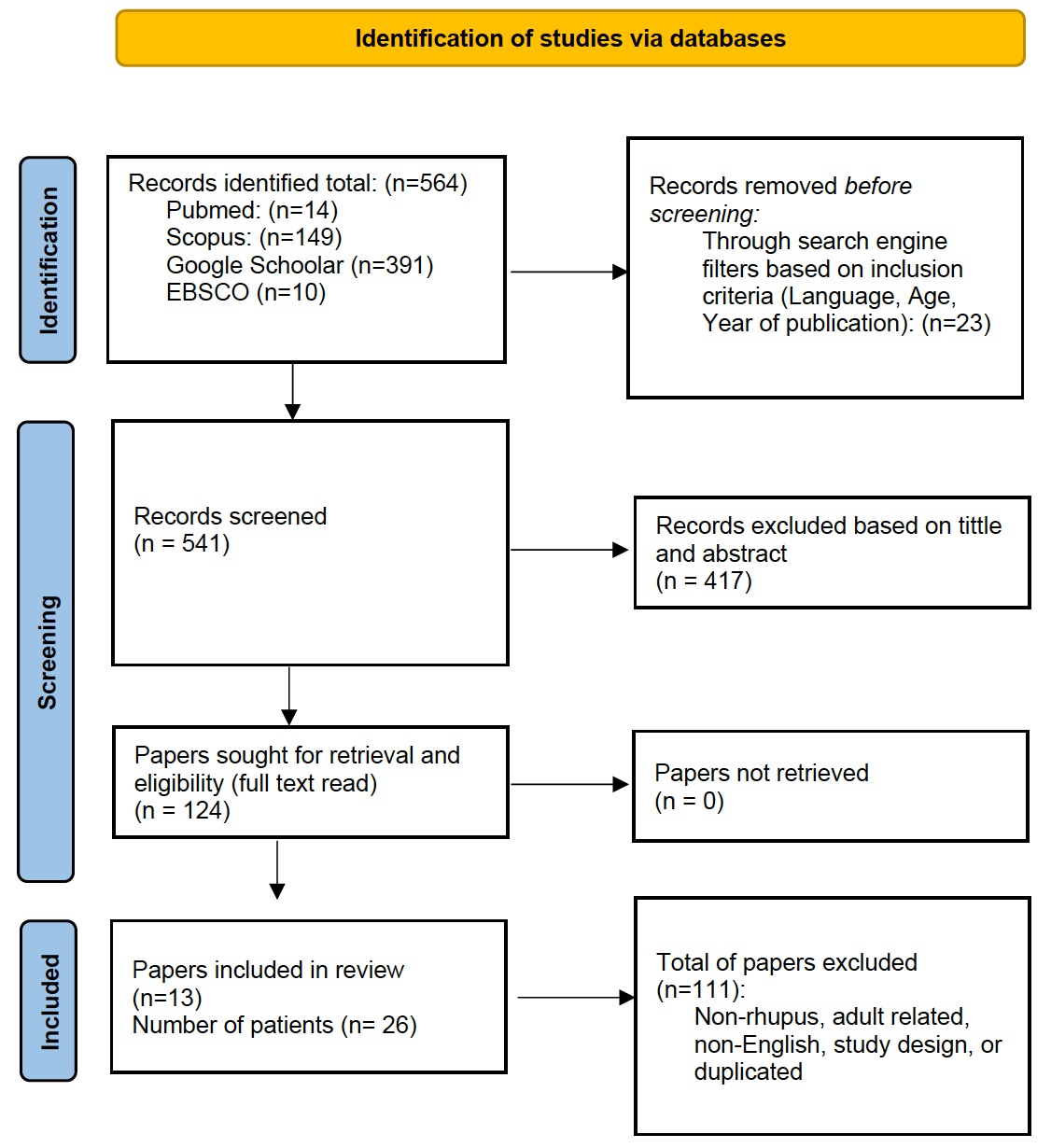 Figure 1. Prisma Flowchart regarding Rhupus diagnostic findings in pediatric patients a Systematic Literature Review
Figure 1. Prisma Flowchart regarding Rhupus diagnostic findings in pediatric patients a Systematic Literature Review
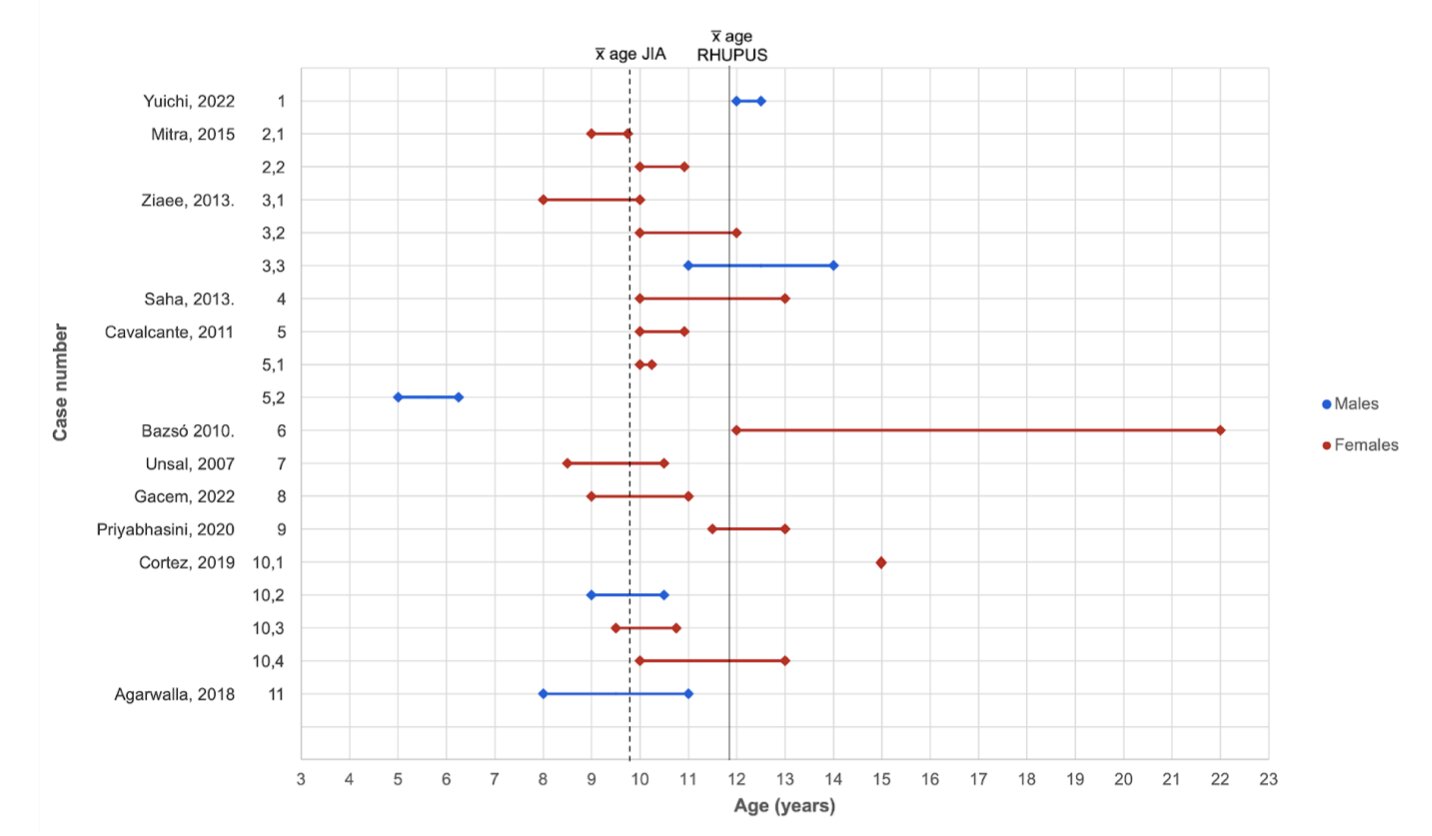 Figure 2. The first diamond shape per case corresponds to the onset of JIA, and the second diamond represents the onset of Rhupus. The dashed line shows the mean age of JIA diagnosis (9 years, 10 months). The full line shows the mean age for the development of Rhupus (10 years, 10 months).
Figure 2. The first diamond shape per case corresponds to the onset of JIA, and the second diamond represents the onset of Rhupus. The dashed line shows the mean age of JIA diagnosis (9 years, 10 months). The full line shows the mean age for the development of Rhupus (10 years, 10 months).
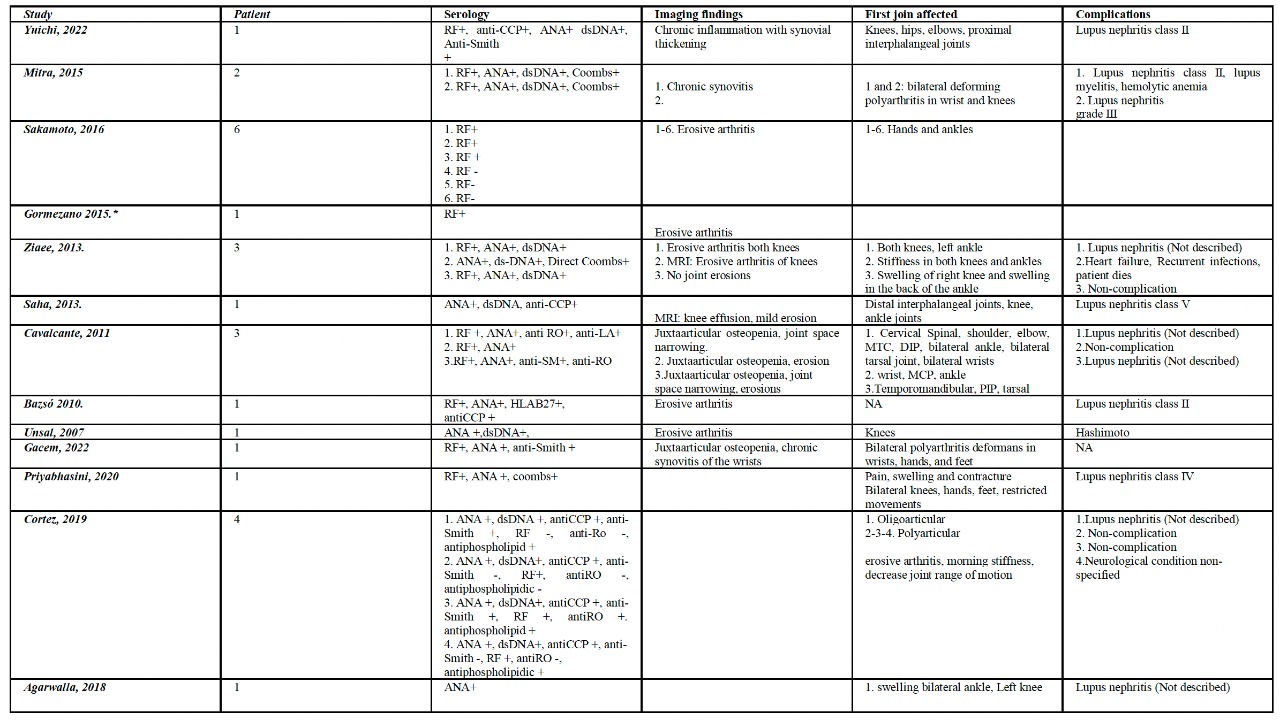 Table 1. Detailed clinical, serology, and imaging findings of pediatric patients with Rhupus
Table 1. Detailed clinical, serology, and imaging findings of pediatric patients with Rhupus
To cite this abstract in AMA style:
Velez M, Nicolalde B, Moreno-Montenegro K, Carrera-Barriga G, Gallegos C, Leon B. Clinical, Serologic, and Imaging Findings of Rhupus Syndrome in the Pediatric Population: A Systematic Literature Review [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/clinical-serologic-and-imaging-findings-of-rhupus-syndrome-in-the-pediatric-population-a-systematic-literature-review/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-serologic-and-imaging-findings-of-rhupus-syndrome-in-the-pediatric-population-a-systematic-literature-review/
