Session Information
Session Type: Poster Session B
Session Time: 5:00PM-6:00PM
Background/Purpose: TM joint arthritis is an underrecognized complication of JIA that can cause long-term problems including decreased mandibular growth, altered facial morphology, and orofacial pain. It is estimated that the TM joint may be affected in 40-80% of children with JIA. Standardized physical exam and imaging are important ways to accurately assess for this phenomenon. Little is known about the rate at which providers evaluate for TM joint involvement in their clinical practice.
Methods: Data was obtained from the New Childhood Arthritis and Rheumatology Research Alliance (CARRA)Registry. Data fields related to assessment for TM joint arthritis were added in 2019. Patients were included in the study if they had a diagnosis of JIA and had data recorded between January 2020 and August2021. Standard descriptive statistics were used to describe demographic and clinical features.
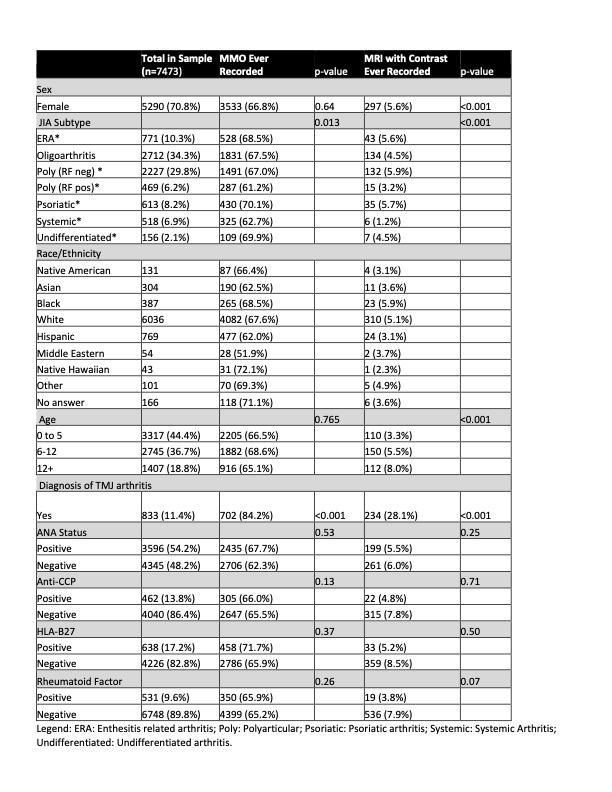
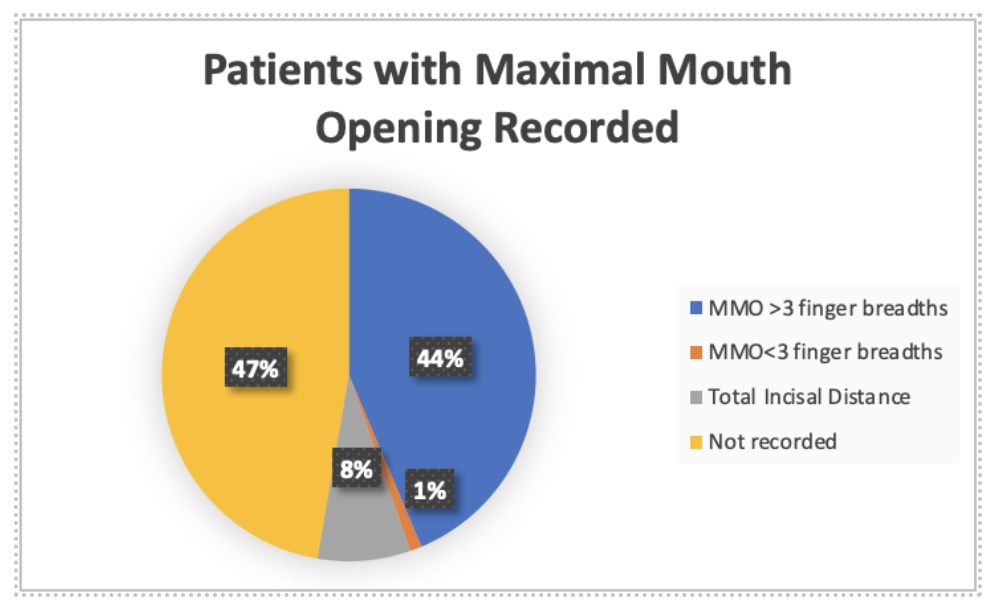
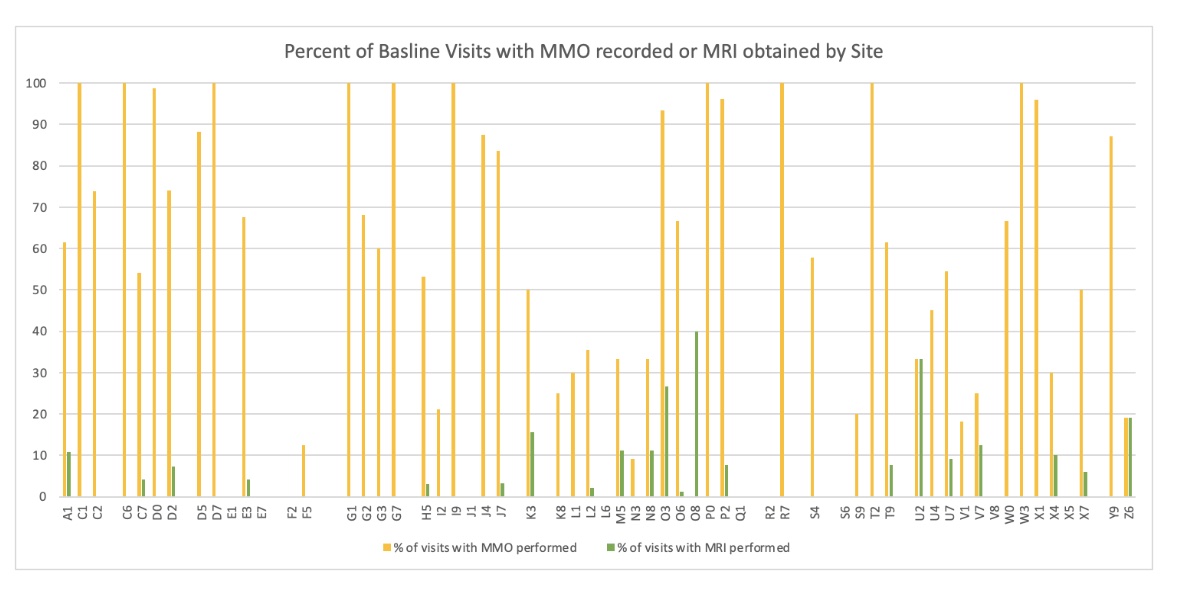
Results: 17761 visits were reviewed for a total of 7473 patients with JIA. 52.7% of patients ever had maximal mouth opening (MMO) recorded as finger breadths or total incisal distance (TID). Only 8% had TID measured (Figure 2). 5.0%had MRI with contrast performed. 939 patients had a diagnosis of TM joint arthritis. Of these, 28.5% have an MRI documented, 83% have an MMO documented, and 40% have TID measured. During the study, 51 patients were newly diagnosed with TM joint arthritis. 84% have MMO recorded which was evaluated as TID in 51%. 41%had an MRI with contrast. Few patient-level characteristics were statistically related to having MMO assessed. It was assessed in ~2/3 of patients in all subtypes (Table 1). MRI was more likely to be obtained in older patients and in female patients. It was significantly more likely that MMO was recorded at the patients baseline visit than at a follow up visit. There was variance in assessments between the 59 sites. MMO was recorded at the baseline visit on 80% of patients at 3 sites and it was never recorded at 11 sites. MRIs were infrequently performed at all sites with 38 sites having no MRIs ordered (Figure 3).
Conclusion: Maximal mouth opening is not consistently measured in patients with JIA, and it is rarely measured quantitatively. Similarly, TMJ MRIs are rarely obtained in these patients. Site of care is more associated with TMJ assessments than patient level characteristics. It is possible that abstractions of TMJ data into the database is incomplete and does not reflect clinical assessment. The data fields were newly added, and it is possible that completion rates might increase in later time periods. However, this data suggests that education of providers is needed to improve the assessment of the TM joint in patients with JIA to help prevent long-term complications.
To cite this abstract in AMA style:
Costello A, Twilt M, Lerman M. Provider Assessment of the Temporomandibular Joint in Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/provider-assessment-of-the-temporomandibular-joint-in-juvenile-idiopathic-arthritis/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/provider-assessment-of-the-temporomandibular-joint-in-juvenile-idiopathic-arthritis/