Session Information
Date: Monday, November 14, 2022
Title: Abstracts: Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes II: Imaging
Session Type: Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Previous studies of patients with axial spondyloarthritis (axSpA) have demonstrated that certain MRI structural lesions in the sacroiliac joints (SIJ), notably erosions, has high specificity for axSpA. However, a recent study has reported a progressive increase in MRI structural lesions in healthy individuals with increasing age, erosions being detected in as many as 40% of those aged ≥401. If replicated in other cohorts, this could have a major impact on the diagnostic interpretation of MRI lesions in the SIJ. We aimed to assess the impact of increasing age on the frequency of MRI lesions in the SIJ in cohorts of healthy individuals without back pain and those diagnosed with non-specific back pain (NSBP).
Methods: We assessed MRI SIJ lesions in 2 independent cohorts: A. 79 healthy volunteers (HV) and 87 with NSBP aged ≤49 years from the staffs of two university hospitals in Canada and Switzerland, the absence of back pain being confirmed using the Nordic Questionnaire, B. 237 patients ≤45 years referred to a rheumatologist with undiagnosed back pain suspicious of axSpA in the ASAS Classification Cohort (ASAS-CC), of whom 69 were diagnosed with NSBP. MRI lesions were assessed on an online interface and recorded in SIJ quadrants or halves of consecutive semicoronal slices through the SIJ. Lesions were ascertained by 5 central readers for cohort A and 7 central readers for cohort B according to standardized lesion definitions (CANDEN for cohort A and ASAS definitions for cohort B) and the results analyzed according to age categories and recently reported, data-driven, MRI cut-offs for a positive MRI indicative of inflammatory or structural lesions typical of axSpA (SIJ+/MRIstructure or SIJ+/MRIinflammation)2.
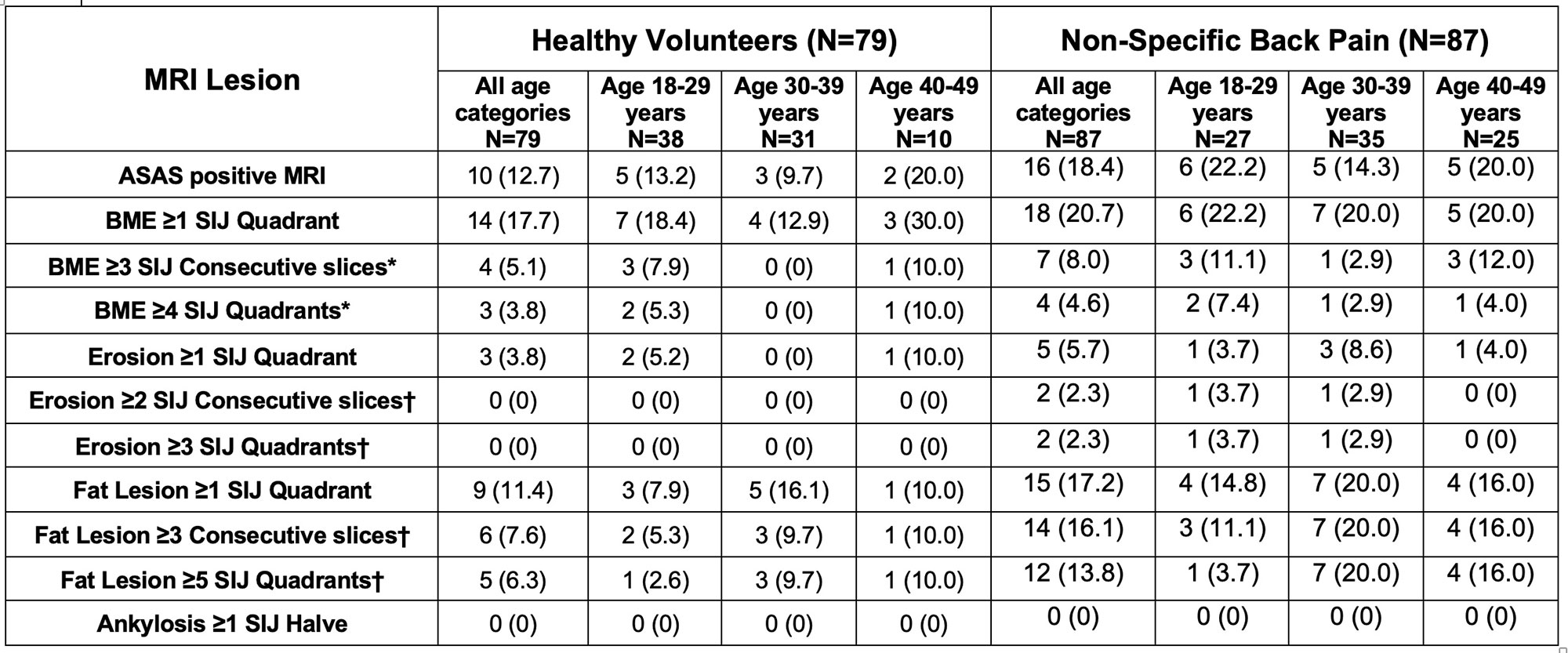
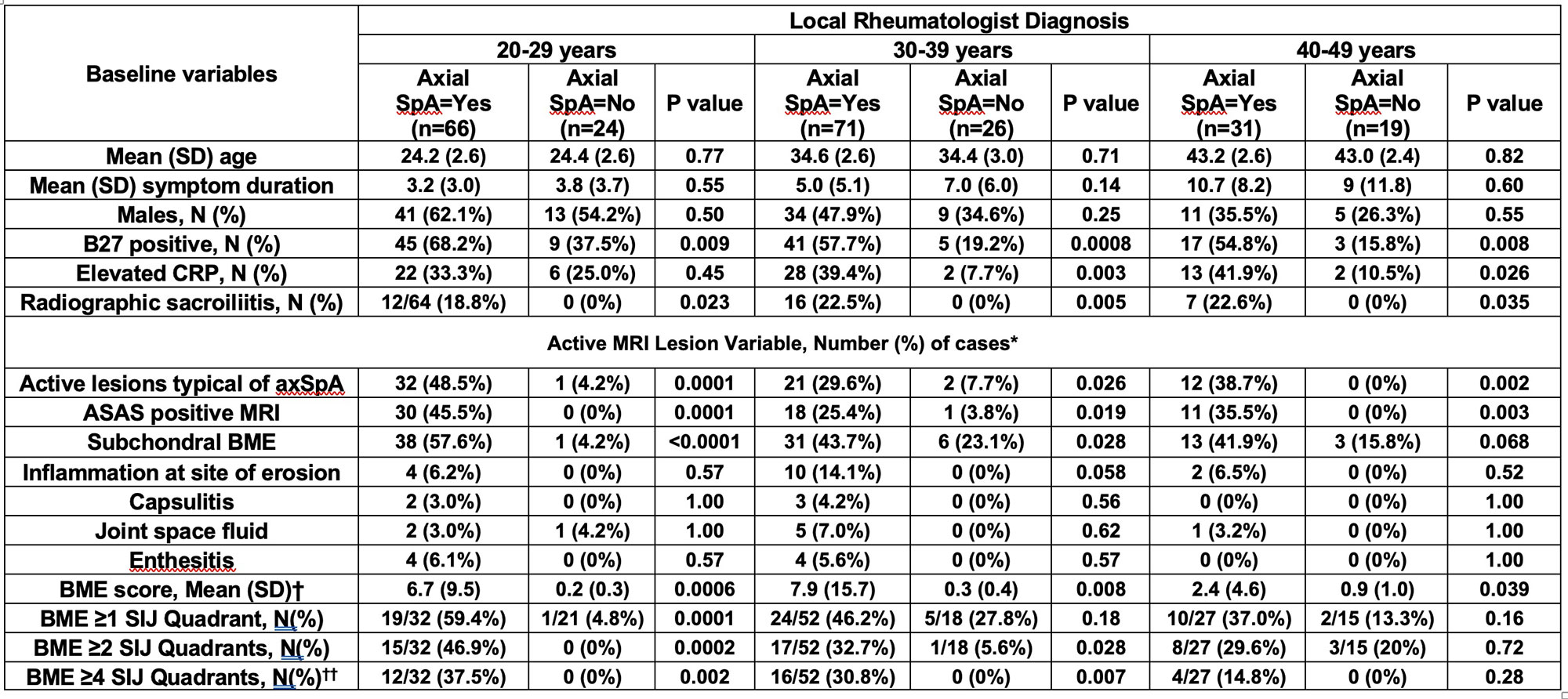
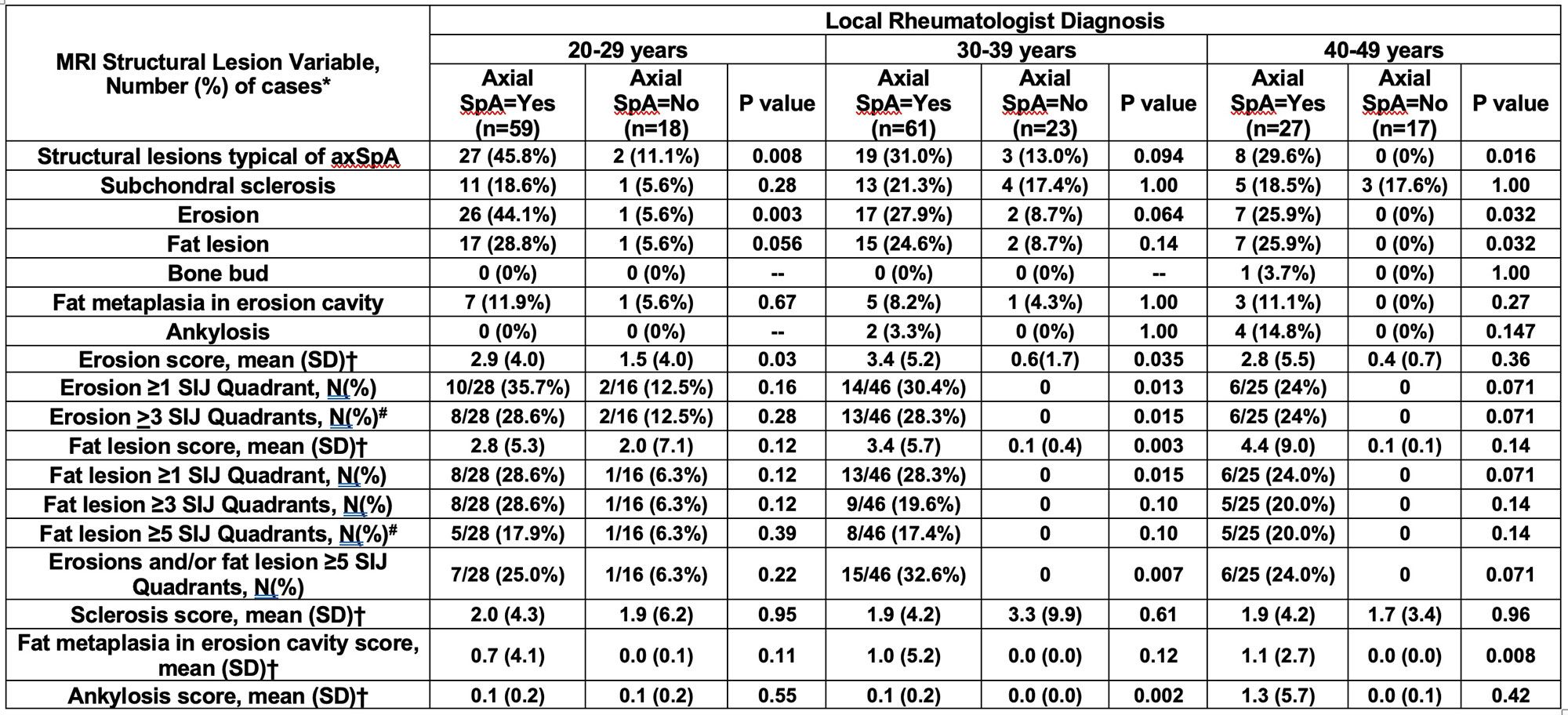
Results: In cohort A (Table 1), the frequencies of BME lesions were higher for HV in the oldest age category (40-49 years), although a progressive increase for NSBP with increasing age was not evident. Only 3/79 (3.8%) of HV and 4/87 (4.6%) of NSBP had BME in ≥4 SIJ quadrants, the cut-off denoting SIJ+/MRIinflammation. Only 3/79 (3.8%) of HV and 5/87 (5.7%) of NSBP had an erosion in ≥1 SIJ quadrant by majority of readers. None of HV and only 2/87 (2.3%) of NSBP had erosion in ≥2 consecutive slices and/or ≥3 SIJ quadrants, the cut-offs denoting SIJ+/MRIstructure. More fat lesions were noted in NSBP than HV but a progressive increase with age was not evident. In cohort B (ASAS-CC), similar frequencies for active and structural lesions were noted in cases with NSBP to cohort A (Tables 2 and 3) and a progressive increase with age was not evident. Moreover, there was not a single case with a SIJ+/MRIstructure in the higher age categories and the finding of erosion was equally discriminatory between axSpA and NSBP, irrespective of age category.
Conclusion: Data from HV and NSBP controls does not indicate progressive increases in MRI structural lesions in the SIJ with increasing age when standardized definitions for reporting axSpA lesions are adopted. MRI cut-offs for a positive MRI indicative of active or structural MRI lesions typical of axSpA discriminate equally well between axSpA and NSBP across age categories.
Ref 1. Renson et al. Arthritis Rheumatol 2022 doi.org/10.1002/art.42145. 2. Maksymowych et al. Rheumatol 2021;60:4778–4789
To cite this abstract in AMA style:
Weber U, Pedersen S, Østergaard M, Machado P, Baraliakos X, Lambert R, Maksymowych W. Relative Frequencies of the Spectrum of MRI Lesions in the Sacroiliac Joints of Healthy Individuals and Patients with Non-Specific Back Pain: What Is the Impact of Increasing Age? [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/relative-frequencies-of-the-spectrum-of-mri-lesions-in-the-sacroiliac-joints-of-healthy-individuals-and-patients-with-non-specific-back-pain-what-is-the-impact-of-increasing-age/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/relative-frequencies-of-the-spectrum-of-mri-lesions-in-the-sacroiliac-joints-of-healthy-individuals-and-patients-with-non-specific-back-pain-what-is-the-impact-of-increasing-age/