Session Information
Date: Monday, November 14, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Pediatric systemic lupus erythematosus (pSLE) is associated with significant morbidity and multiorgan dysfunction. Single-center studies have described disease activity and damage trajectories for pSLE, which varied by self-reported ethnicity and did not include measures of socioeconomic status. We utilized data from the Childhood Arthritis and Rheumatology Research Alliance (CARRA) Registry to 1) describe 2-year trajectories of disease activity as measured by the Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI 2K); 2) identify key baseline patient characteristics associated with different trajectories; and 3) compare clinical characteristics and treatments among different trajectories at 24 months of enrollment.
Methods: Participants were included if they had a diagnosis of SLE within 12 months of baseline visit. Exclusion criteria included having ≤ 2 Registry visits and secondary rheumatologic conditions. Baseline sociodemographic (including the Area Deprivation Index (ADI)), clinical, and treatment characteristics were included in modeling. The SLEDAI 2K was calculated at 6-month visits. Latent trajectory analysis (LTA) was performed with the maximum likelihood method to account for missing data. Within each model, the posterior probability of being assigned to each trajectory was calculated. Patients were then assigned to the trajectory of highest probability. Associations between trajectory groups and patient characteristics were assessed with descriptive statistics and multinomial generalized logistic regression modeling using multiple imputation for missing data.
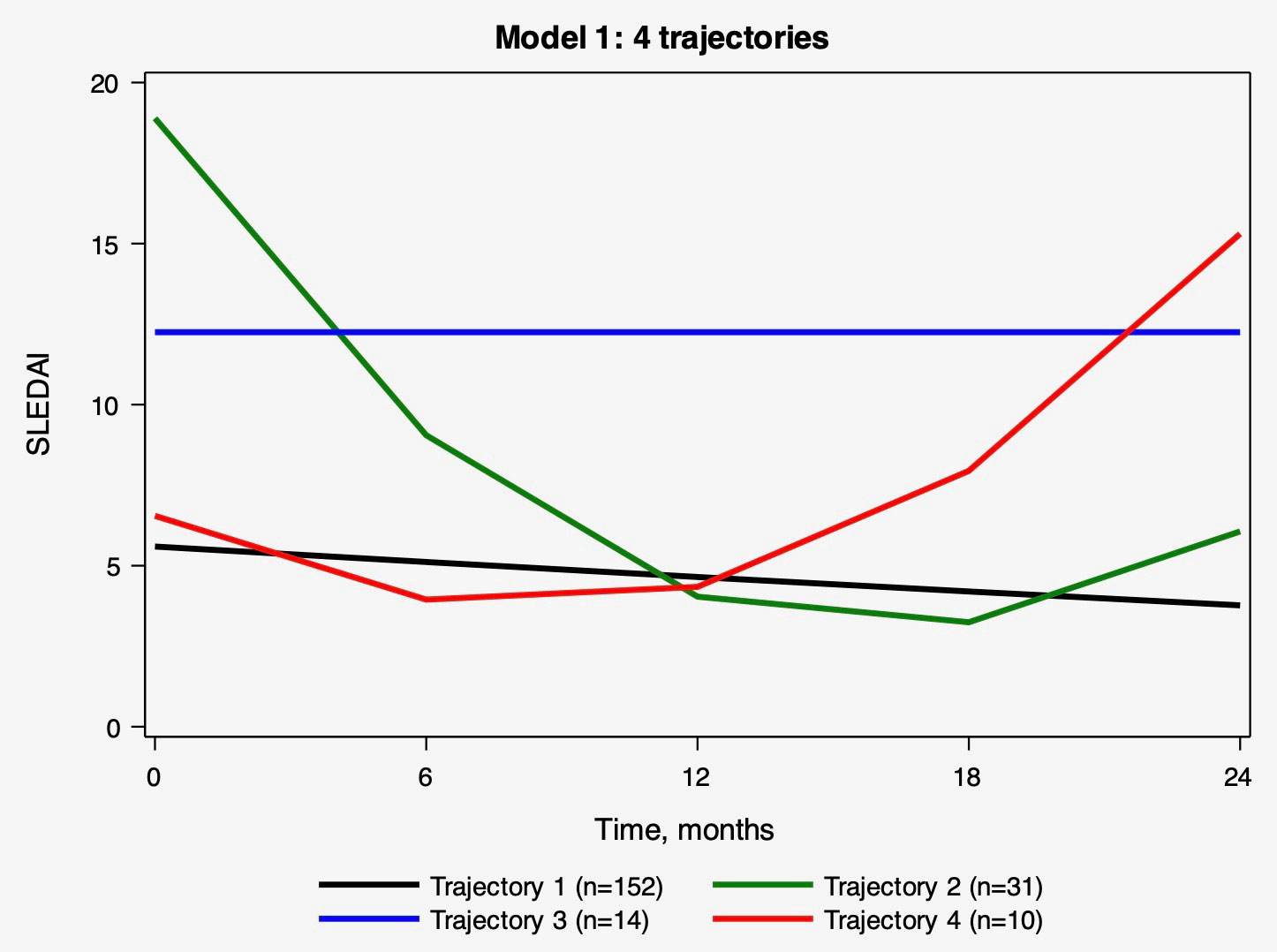
Results: 207 patients were included in the LTA. The BIC, AIC, and average posterior probabilities are presented for the top model of SLEDAI 2K trajectories (Table 1) and shown over time (Figure 1). Trajectories of SLEDAI 2K scores included T1) low and stable, T2) high and decreasing, T3) intermediate and stable, and T4) low and increasing. Baseline characteristics significantly differed between trajectories for insurance, ADI, time from diagnosis to baseline visit and multiple disease activity and damage measurements (Table 2). The multinomial generalized logistic regression considered the same variables for inclusion. Only time from diagnosis to baseline (per 10 days) (OR 1.01 (95% CI 1.00-1.03) comparing T3 and T1) and baseline SLEDAI score (OR 2.41 (95% CI 1.70-3.41) comparing T2 and T1, and OR 1.43 (95% CI 1.21-1.69) comparing T3 and T1) remained significant. These variables were also predictive of trajectory membership at 24 months, along with physician global assessment and use of mycophenolate mofetil and azathioprine.
Conclusion: In a diverse cohort of patients with active pSLE, we identified distinct disease activity trajectories that were predicted by time from diagnosis to baseline registry visit and baseline SLEDAI 2K score. There were no significant differences between trajectories for self-identified race or ethnicity, ADI, or baseline medication use. Given the known relationship between disease activity and damage, pSLE patients with high SLEDAI 2K scores at baseline visit should be closely monitored for persistent or worsening disease activity.
To cite this abstract in AMA style:
Case S, Hill L, Dennos A, Phillips T, Schanberg L, von Scheven E, Knight A, Hersh A, Son M. Trajectories of Disease Activity in a Longitudinal Registry of Pediatric SLE [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/trajectories-of-disease-activity-in-a-longitudinal-registry-of-pediatric-sle/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trajectories-of-disease-activity-in-a-longitudinal-registry-of-pediatric-sle/