Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Frailty is increasingly recognized among individuals living with RA. While several tools are available to assess frailty in clinical settings, it is less readily measured in administrative health datasets. Our aim was to develop and evaluate a frailty index (FI) for individuals with RA using administrative health data.
Methods: We conducted a population-based cohort study using administrative health data for a Canadian province from 1990 – 2018. A previously validated case definition based on physician billing data was used to assemble an incident cohort of all cases with RA onset from 1996 – 2008. To capture the health state of individuals living with RA, the baseline date was defined as 5 years after the index date for RA diagnosis. We randomly sampled 50% of the incident RA cohort for FI derivation, while the remaining 50% was used for FI validation.
Health deficits for the FI were selected using published criteria. First, 101 candidate variables were identified via literature review and evaluated in the derivation cohort for data availability, prevalence, and relationship with age. Next, 60 eligible variables were evaluated by an expert panel in a modified Delphi consensus process. Participants ranked each candidate variable’s association with adverse outcomes (0-9) and overall suitability (0-9). Forty health deficits met criteria for inclusion in the FI, which required median scores ≥ 7 with no disagreement. Each deficit was scored from 0 (absent) to 1 (present) and individual deficit scores were combined to produce a baseline FI score for each patient.
We evaluated the association of baseline FI scores with health outcomes during follow-up, including mortality, acute care hospitalizations, and emergency department (ED) visits. Follow-up began on the baseline date and continued until the earliest occurrence of death, leaving the province, or the end of the study period. Mortality risk was modelled using Cox regression, while negative binomial regression was used to model the rates of hospitalizations and ED visits during follow-up. Predictive accuracy of the FI was compared to the Romano version of the Charlson comorbidity index (CCI). Multivariable models were adjusted for age, sex, rurality, and socioeconomic status.
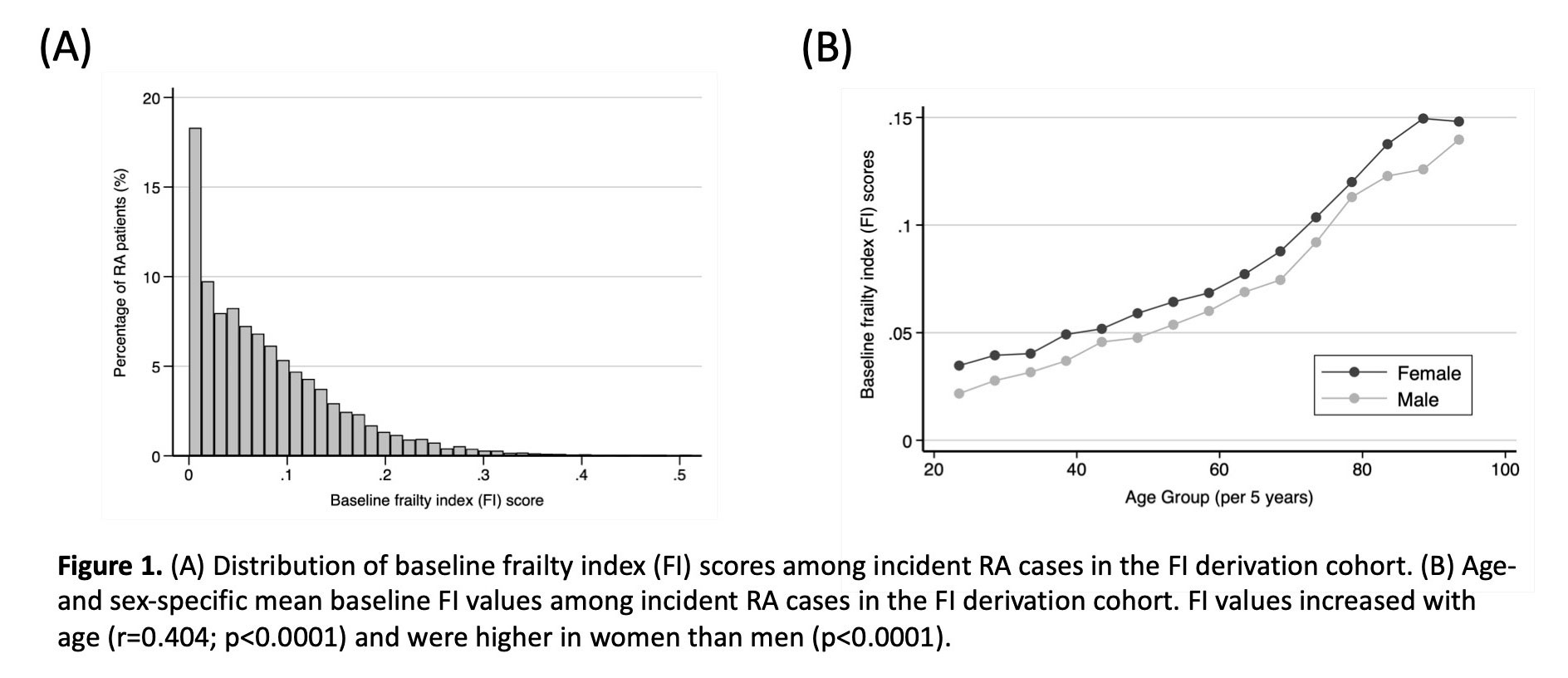
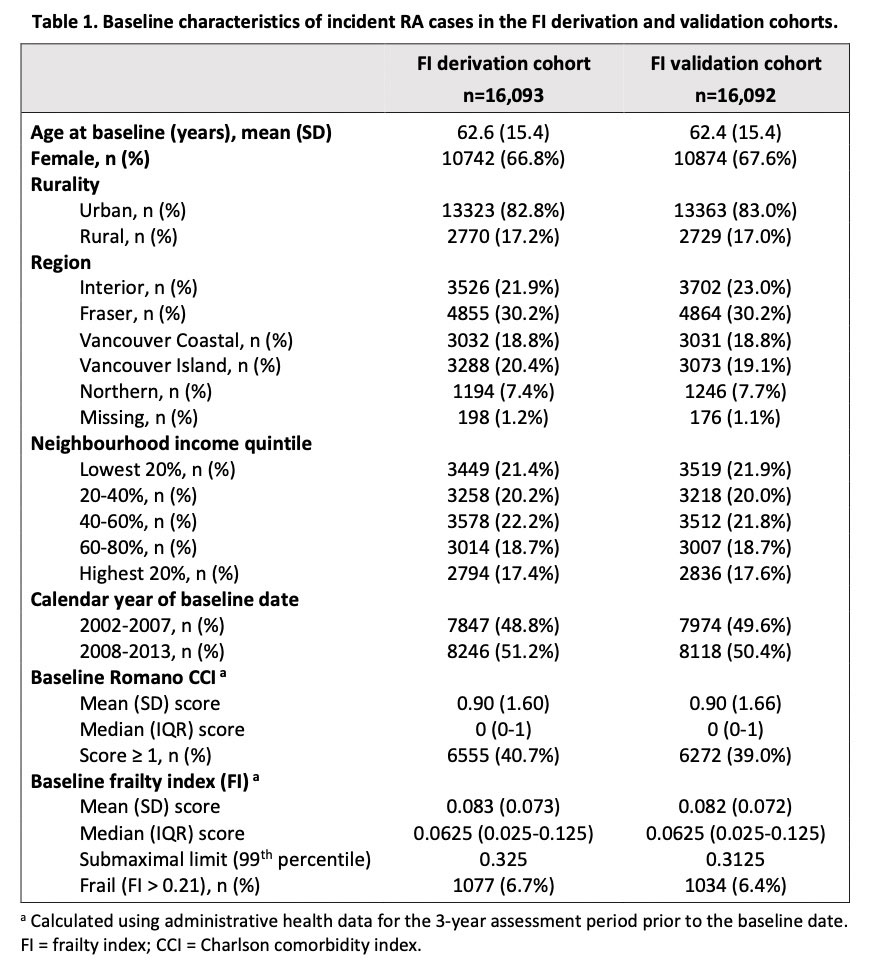
Results: Baseline characteristics for the derivation cohort (n=16093) and the validation cohort (n=16092) are shown in Table 1. In the derivation cohort, the distribution of baseline FI scores was right-skewed (Figure 1a), with 7% of RA patients classified as frail (FI > 0.21). FI scores increased with increasing age (Figure 1b). Baseline FI scores were associated with mortality risk and rates of hospitalizations and ED visits during follow-up (Table 2). The FI was similar to the CCI for predicting mortality, but superior for predicting hospitalizations and ED visits. Addition of the FI to existing measures improved outcome prediction. FI performance was similar in the validation cohort (Table 2).
Conclusion: The FI quantifies risk of adverse health outcomes that is not otherwise captured by demographic variables and traditional comorbidity measures in administrative health data. With further validation, the FI is a promising tool for understanding the impact of frailty on health outcomes in RA.
To cite this abstract in AMA style:
Legge A, Lacaille D. Using Administrative Health Data to Construct a Frailty Index as a Measure of Susceptibility to Adverse Health Outcomes Among Individuals with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/using-administrative-health-data-to-construct-a-frailty-index-as-a-measure-of-susceptibility-to-adverse-health-outcomes-among-individuals-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/using-administrative-health-data-to-construct-a-frailty-index-as-a-measure-of-susceptibility-to-adverse-health-outcomes-among-individuals-with-rheumatoid-arthritis/