Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: The prevalence of rheumatoid arthritis (RA) in persons 60 years or older is estimated to be 2%. Late onset rheumatoid arthritis (LORA) is a sub-group of patients traditionally defined as onset of RA after the age of 60 years. Compared to younger onset rheumatoid arthritis (YORA) which occurs before the age of 60 years, LORA has unique characteristics and disease manifestations. The prognosis of LORA patients is less clear based on prior studies. We compared the clinical characteristics, time to remission and treatment regimen at remission between LORA and YORA patients.
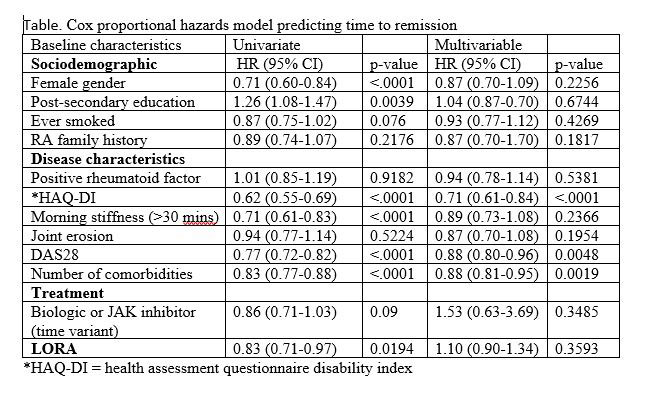
Methods: The Ontario Best Practices Research Initiative (OBRI) is a clinical registry of RA patients followed in routine care. This analysis used the OBRI database from 2008 to 2020. Patients were included if they had active RA disease (≥1 swollen joint) and were enrolled in the study within 1 year of diagnosis. LORA was defined as diagnosis of RA after age of 60, YORA as under age of 60. Remission was defined by Disease Activity Score 28 (DAS28) ≤2.6. A multivariable Cox proportional hazards model was used to estimate time to remission.
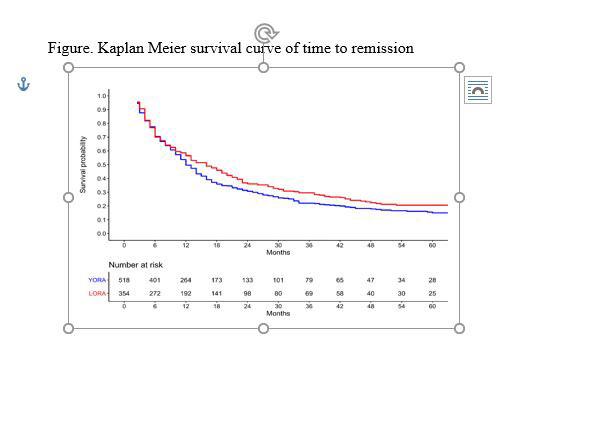
Results: The study included 354 LORA patients and 518 YORA patients. Compared to YORA patients, LORA patients were less likely to be female (66% vs. 80% p< 0.0001), and less likely to have positive either rheumatoid factor or anti-cyclic citrulinated peptide antibody (63% vs. 75% p=0.0003). The mean (standard deviation) baseline DAS28 score was 5.0 (1.3) and 4.8 (1.2) in LORA and YORA patients, respectively (p=0.0946). During the study follow-up, 254 (72%) LORA and 405 (78%) YORA patients reached remission (Figure). Compared to YORA patients, the hazard ratio (HR) for remission in LORA patients was 1.10 (95% confidence interval 0.90 to 1.34 p=0.35) after adjusting for other prognostic factors (table). For patients who reached remission, LORA patients were less likely to be on a biologic or JAK inhibitor (16% vs. 27%) and more likely to be on a single conventional synthetic disease-modifying anti-rheumatic drugs (csDMARD) (34% vs. 27%) compared to YORA patients (chi-square test for all drug groups p=0.0039).
Conclusion: LORA and YORA patients had similar prognosis in terms of time to remission. At remission, LORA patients were more likely to be on a single csDMARD without a biologic or JAK inhibitor. Clinicians should take the same approach for all RA patients targeting remission regardless of age of onset.
Reference:
Ruban TN, Jacob B, Pope JE, Keystone EC, Bombardier C, Kuriya B. The influence of age at disease onset on disease activity and disability: results from the Ontario Best Practices Research Initiative. Clinical rheumatology. 2016 Mar;35(3):759-63.
To cite this abstract in AMA style:
Li X, Cesta A, Movahedi M, Bombardier C. Late Onset Rheumatoid Arthritis Has a Similar Remission Rate as Younger Onset Rheumatoid Arthritis: Results from an Ontario Rheumatoid Arthritis Registry [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/late-onset-rheumatoid-arthritis-has-a-similar-remission-rate-as-younger-onset-rheumatoid-arthritis-results-from-an-ontario-rheumatoid-arthritis-registry/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/late-onset-rheumatoid-arthritis-has-a-similar-remission-rate-as-younger-onset-rheumatoid-arthritis-results-from-an-ontario-rheumatoid-arthritis-registry/