Session Information
Date: Sunday, November 13, 2022
Title: Vasculitis – ANCA-Associated Poster II: Treatment Efficacy, Clinical Outcomes, Biomarkers
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Anti-neutrophil cytoplasmic antibody-associated vasculitis (AAV) is an autoimmune disease that can involve various organs systematically. Kidney involvement, one of the major manifestations of AAV, presents with urinary abnormalities including hematuria and proteinuria, and is associated with the risk of chronic kidney disease (CKD). Despite the significance of persistent hematuria in AAV, the clinical value of proteinuria in the clinical course of AAV remains unknown. Therefore, we aimed to determine the prognostic significance of proteinuria monitoring in patients with AAV.
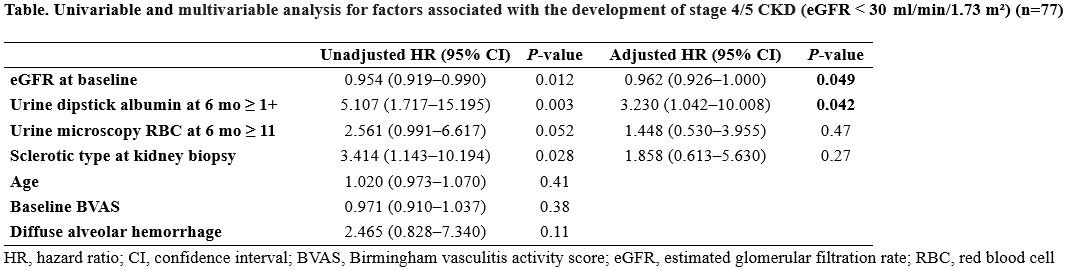
Methods: We retrospectively analyzed the data of patients who were diagnosed with AAV from March 2004 to August 2021 at a single tertiary center in Seoul, Korea. Kidney involvement of AAV was confirmed using kidney biopsy results. Birmingham Vasculitis Activity Score version 3.0 was used to evaluate the disease activity. Proteinuria was evaluated by a urine dipstick test. Poor renal outcome was defined as stage 4/5 CKD (estimated glomerular filtration rate [eGFR] < 30 ml/min/1.73 m2).
Results: A total of 77 patients with a median follow-up duration of 36 months (interquartile range, 18–79) were included in the study. Of them, 65 (84.4%) achieved remission after induction therapy. The patients were divided into two groups according to the presence of proteinuria at 6 months after induction therapy (n = 36 with proteinuria, 41 without proteinuria). After the remission of AAV, 13 of 65 patients relapsed, and there was no significant difference in the rate of relapse or death according to the presence of proteinuria (p=0.447 for relapse, 0.312 for death). In contrast, patients with proteinuria had significantly lower kidney function than did those without proteinuria (31 vs. 45 ml/min/1.73m², p=0.001). Multivariate analysis revealed that baseline kidney function (hazard ratio [HR], 0.962; 95% CI, 0.926–1.000, p=0.049) and proteinuria at 6 months (HR, 3.230; 95% CI, 1.042–10.008, p=0.042) were significantly associated with the development of stage 4/5 CKD.
Conclusion: The presence of proteinuria at 6 months after induction therapy and low renal function at baseline were significantly associated with the risk of severe CKD in patients with AAV. Monitoring for proteinuria after induction therapy may be helpful in predicting poor renal outcomes in patients with AAV.
To cite this abstract in AMA style:
lee Y, Ahn S, Oh J, Kim Y, Lee C, Yoo B, Hong S. Prognostic Value of Proteinuria Monitoring in Anti-neutrophil Cytoplasmic Antibody-associated Vasculitis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/prognostic-value-of-proteinuria-monitoring-in-anti-neutrophil-cytoplasmic-antibody-associated-vasculitis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prognostic-value-of-proteinuria-monitoring-in-anti-neutrophil-cytoplasmic-antibody-associated-vasculitis/