Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: A health disparity exists for AA women with SLE who have increased morbidity & mortality from both cervical cancer & SLE. Current cervical cancer screening guidelines are inadequate for these women who need frequent monitoring. We pilot tested a self-sampling brush to obtain cervical cytology & study HPV genetics to develop a less expensive & more convenient way to make cervical cancer screening more accessible for these high risk women
Methods: 30 AA women with SLE recruited from the Rheumatology clinics consented to participate in the study (IRB approved by Ascension St. John Hospital IRB). Inclusion criteria: AA women with SLE, ages 18-50 years, able to consent and obtain vaginal self sampling. Exclusion criteria: current pregnancy, & not meeting inclusion criteria. Clinical information was obtained by records review & interviewing the patient, & surveys administered to assess cervical health information, knowledge of HPV, and satisfaction with using the self sampling brush. Vaginal self sampling by the participant was performed after instruction & the brush immersed in an RNA-stable ThinPrep vial. Hologic ThinPrep automated processor was used for slide preparation & cytology read by a board-certified cytopathologist. HPV DNA &RNA were extracted, & samples were frozen at -80 0C for further analysis.
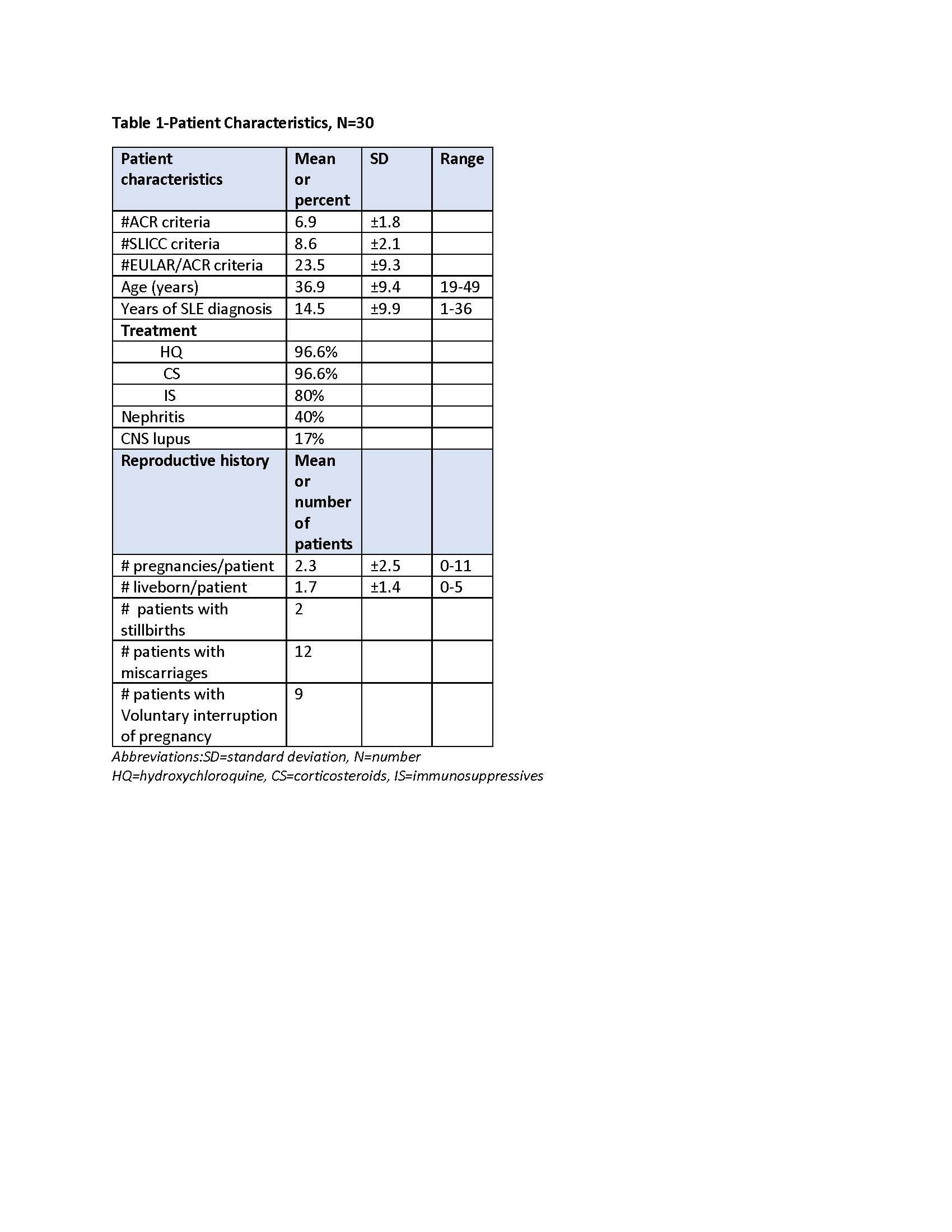
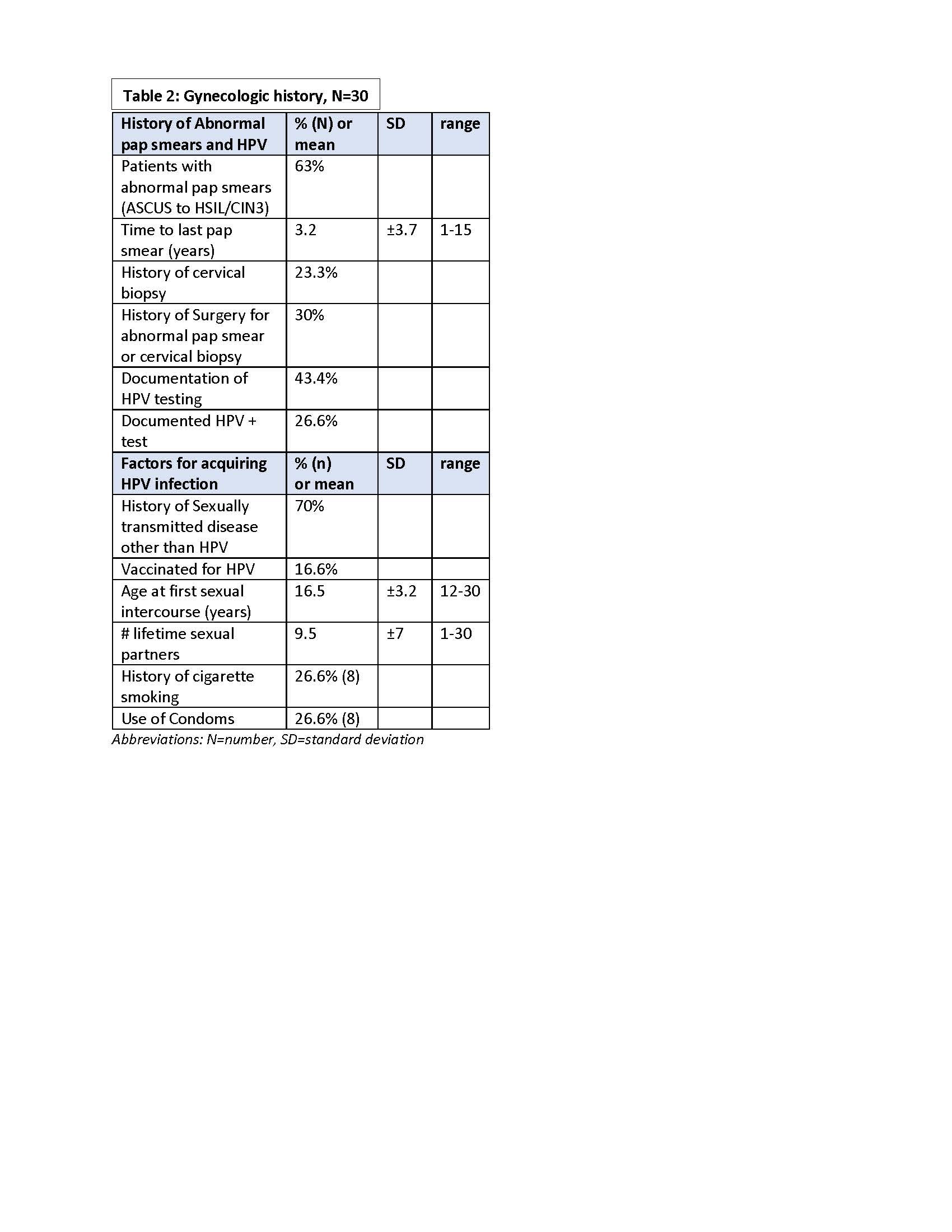
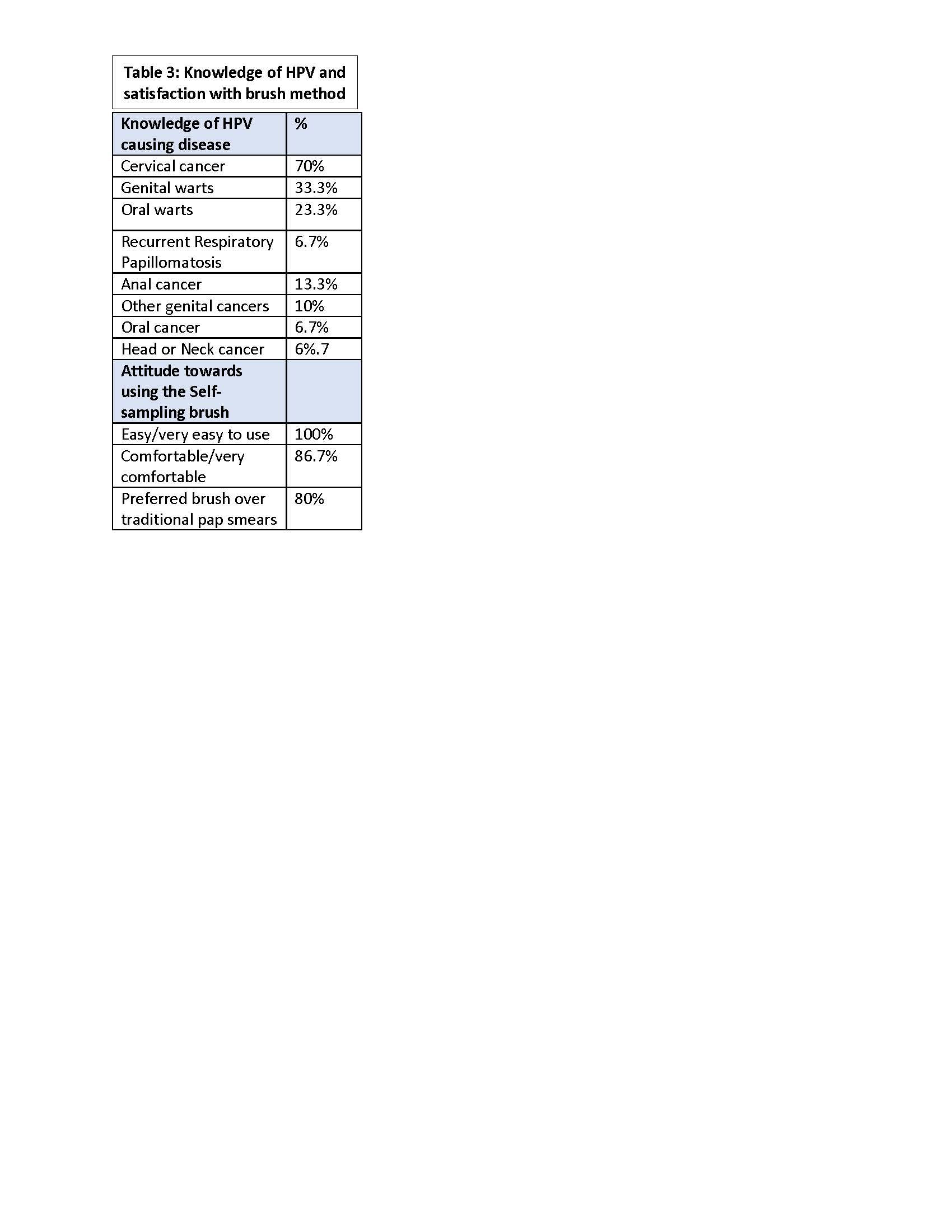
Results: All patients met established criteria for SLE: mean age =36.9 yrs., 40% had lupus nephritis, & all treated with chronic immunosuppressives [Table 1]. Two thirds had a history of abnormal pap smear ranging from atypical squamous sells of undermined significance (ASCUS) to high grade squamous intra-epithelial lesion (HSIL)/cervical intra-epithelial lesion 3 (CIN 3); 7 had a cervical biopsy & 6 underwent a surgical procedure for abnormal cytology or genital warts. HPV test results were available in 43% of which 8 were positive.Most participants had sexually transmitted diseases other than HPV, were not vaccinated for HPV, had multiple lifetime sex partners, did not smoke, & did not use condoms. The average time to last pap smear was 3.2 yrs.[Table 2] Most had knowledge that HPV can cause cervical cancer, but were unaware of HPV causing oral & genital cancers & warts. Most felt the device was easy to use, comfortable, & preferred it for over traditional pap smear. [Table 3].Cytology samples obtained from the brush showed preservation of morphology, but quality indicators were generally absent with abnormal findings in 4/30 : 3=low grade squamous intra-epithelial lesion (LSIL) and 1=ASCUS. Participants were notified of abnormal results & advised to see a gynecologist.
Conclusion: Our high risk cohort had histories of adverse cervical health, yet lacked knowledge about the spectrum of HPV related genital & oral disease & were not following health prevention strategies to reduce their risk with HPV vaccination and condoms. Cervical cytology can be performed using a brush self sampling method of collection. This study highlights the need for cervical health education, increased monitoring & intervention in these high risk women.
To cite this abstract in AMA style:
Dhar J, Walline H, Fathallah L, Szpunar S, Saravolatz L, Mor G, Carey T. Pilot Study: A Novel Method for Cervical Health Monitoring in African American Women with Systemic Lupus Erythematosus (SLE) Using a Self- Sampling Brush to Assess Cervical HPV Infection and Cervical Cytology [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/pilot-study-a-novel-method-for-cervical-health-monitoring-in-african-american-women-with-systemic-lupus-erythematosus-sle-using-a-self-sampling-brush-to-assess-cervical-hpv-infection-and-cervical/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pilot-study-a-novel-method-for-cervical-health-monitoring-in-african-american-women-with-systemic-lupus-erythematosus-sle-using-a-self-sampling-brush-to-assess-cervical-hpv-infection-and-cervical/