Session Information
Date: Saturday, November 12, 2022
Title: Abstracts: SLE – Diagnosis, Manifestations, and Outcomes I: Renal Aspects
Session Type: Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Patients with SLE have an increased risk of developing venous thrombo-embolism (VTE) based on several cohort studies, accounting for significant morbidity and mortality. Lupus nephritis (LN) has been proposed as an independent risk factor for VTE due to the cytokine mediated endothelial damage triggered in SLE and particularly LN.
The aim of this study was to: 1- determine the prevalence of VTE in LN; and 2- study associated risk factors with VTE that may inform clinical practice
Methods: This is a retrospective analysis of all patients followed at the Lupus Clinic who had a diagnosis of LN. Patients were diagnosed with LN based on 24-hour urine proteinuria > 0.5 g/24 hours, spot urinary protein/creatinine ratio (UPCR) > 0.5 g/g, urinary protein greater than 3+ by dipstick analysis or biopsy-proven LN. From the LN cohort, patients with VTE at any point in follow-up were identified, defined as deep vein thrombus (DVT) in the lower extremities, pulmonary embolism (PE) or other vein thrombus.
Patients with VTE after diagnosis of LN were included in further analyses. VTE patients were matched with non-VTE patients by time to VTE and time to last visit available in the data (for non-VTE patients) from LN diagnosis in a nested 1:3 case-control design. Descriptive statistics compared risk factors amongst VTE and matched non-VTE patients. Conditional logistic regressions were conducted to study the association with risk factors of VTE.
Results: Amongst 2093 patients in the SLE database, 1031 were diagnosed with LN (49.3%). 109 of 1031 (10.4%) LN patients developed VTE at any time during follow-up. Of these patients 85 (78.0%) presented with a DVT in the lower extremity, 21 (19.3%) with a PE and 3 (2.7%) with another vein embolism. 52 of 974 patients (5.3%) were diagnosed with VTE after LN diagnosis and included in the nested case-control study, with mean time to VTE of 7.5 years (SD 6.9).
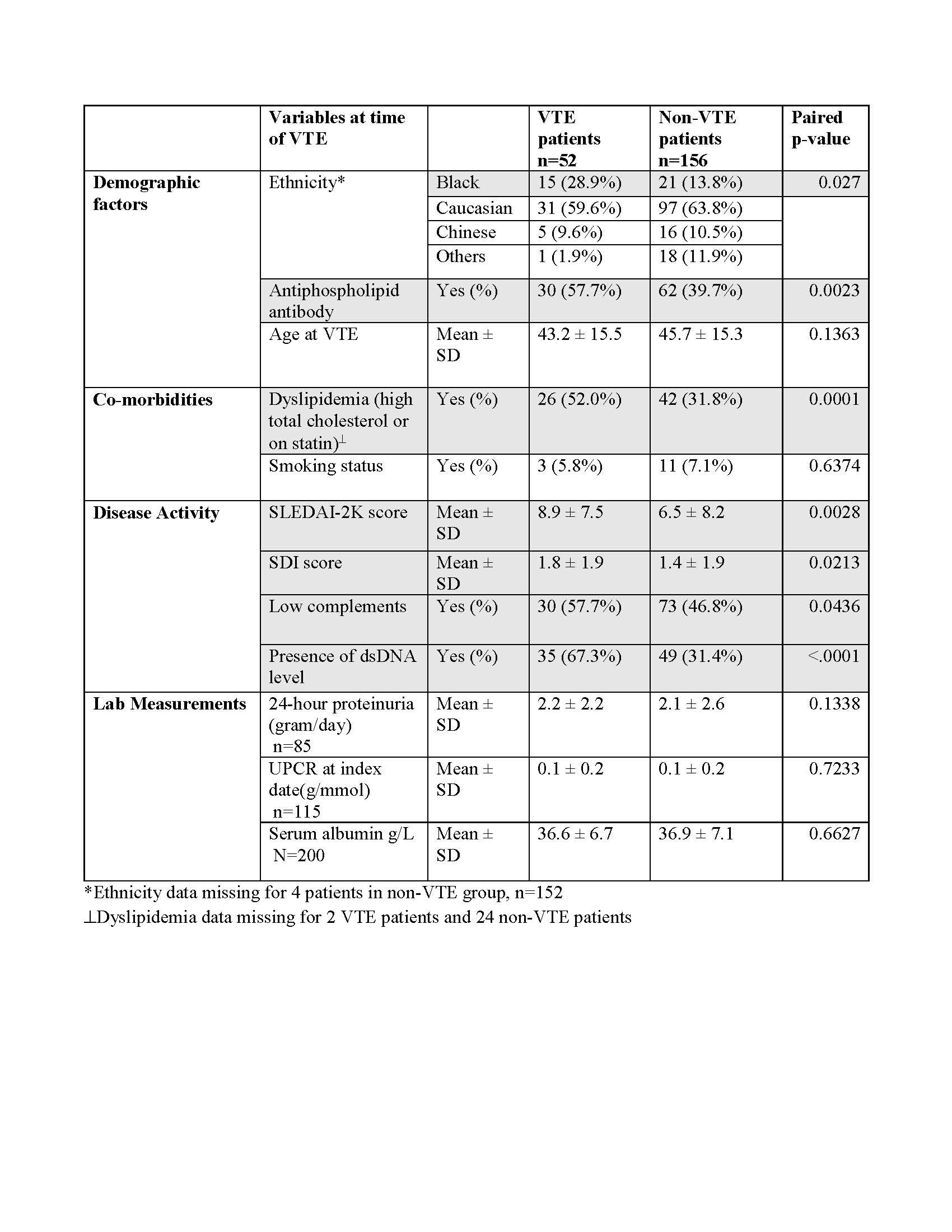
VTE was more common amongst patients who identified as Black (28.9% in VTE group vs. 13.8% in non-VTE group, p=0.027). VTE was more common in those with positive dsDNA (p=< 0.0001), low complements (p=0.044), high SDI (p=0.021), and high SLEDAI-2K (p=0.0028) scores at time of VTE (see Table 1). Antiphospholipid positivity (p=0.0023) and presence of dyslipidemia (p=0.0001) at time of VTE also accounted for statistically significant differences between groups. There were no differences based on UPCR, serum albumin, or 24-hour proteinuria at time of VTE between both groups.
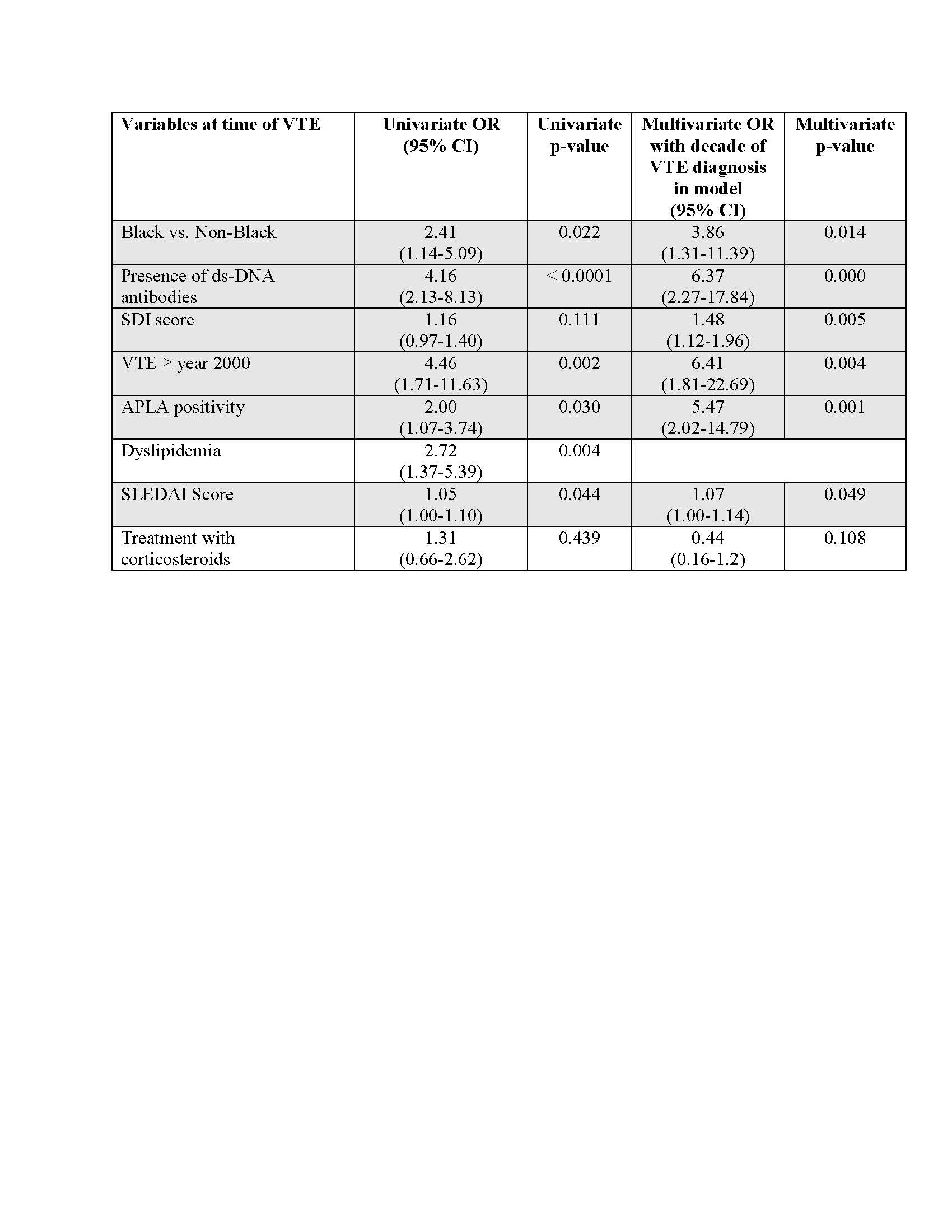
Conditional logistic analyses with index decade (VTE diagnosis) in the model revealed Black ethnicity (OR 3.86, p=0.014), SDI (OR 1.48, p=0.005), SLEDAI-2K (OR 1.07, p=0.049), presence of dsDNA (OR 6.37, p=0.000), and APLA positivity (OR 5.47, p=0.001), were predictive of VTE (see Table 2).
Conclusion: VTE occurred in approximately 10% of LN patients. VTE was more common in individuals with dsDNA, low complements, and higher SLEDAI-2K and SDI, reflecting higher disease activity burden and damage. Regression analyses revealed Black ethnicity, presence of dsDNA, APLA positivity, SDI and SLEDAI-2K scores to be associated with VTE, potentially informing follow-up and clinical care.
To cite this abstract in AMA style:
Tofighi T, Su J, Touma Z. Prevalence of Venous Thrombo-Embolism in Lupus Nephritis and Associated Risk Factors [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-venous-thrombo-embolism-in-lupus-nephritis-and-associated-risk-factors/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-venous-thrombo-embolism-in-lupus-nephritis-and-associated-risk-factors/