Session Information
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: The pediatric rheumatology workforce faces a critical shortage. The recent ACR Pediatric Rheumatology Workforce Study projects that by 2030, modest expansion of the 300 existing providers will be unable meet a twofold excess demand.1 One way to address the workforce gap is to train physicians with dual residency in both medicine and pediatrics (MP) who are prepared to treat populations in child- and adulthood. We explored career paths of the MP residency trained rheumatology workforce to better understand how to improve access to rheumatology care for patients < 18 years of age.
Methods: We used a mixed-methods approach of primary and secondary data to identify and survey the MP residency trained rheumatology workforce. We recruited 1) ABIM certified rheumatologists, 2) ABP certified rheumatologists, 3) ACR members, and 4) a compiled list derived from adult and/or pediatric rheumatology fellowship program directors. From 4/2021-6/2021, an email survey that characterized training background, career path, and demographics was administered by the ACR Committee on Training and Workforce Issues Medicine-Pediatrics workgroup. 144 MP residency trained attending and fellow rheumatologists were identified, with a survey response rate of 46% (66/144). 59 were attending rheumatologists. Data were summarized with descriptive statistics.
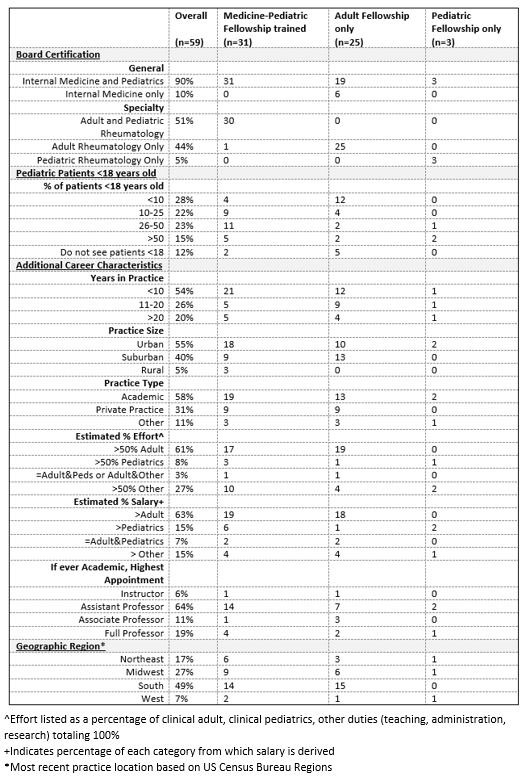
Results: Of 59 respondents, more than half (53%) were trained in combined adult and pediatric rheumatology, 42% in adult rheumatology only, 5% in pediatric rheumatology only Table 1. 90% were board certified in both adult and pediatric medicine and 51% were board certified in both adult and pediatric rheumatology. 88% of respondents treated patients < 18 years old. 64% noted that care of children comprised >25% of their practice. The majority (54%) had less than 10 years of post-fellowship work experience. The majority worked in urban (55%) and/or academic settings (58%) and had salary support from adult medicine (60%). The density of MP trained rheumatologists was greatest in the US South.
Conclusion: Most MP residency-trained rheumatologists cared for pediatric-aged patients; although only 51% became board certified in pediatric rheumatology leading to a loss of potential pediatric rheumatology specialists. One way to address workforce shortages in pediatric rheumatology is to identify and mitigate barriers to career paths for MP residency trained rheumatologists who aim to care for patients < 18 years of age.
1Correll C, et al. Arthritis Care Res. 2022;74:340-348
To cite this abstract in AMA style:
DeQuattro K, Edens C, Herndon C, Marston B, Jonas B. Few and Far Between: Addressing the Pediatric Rheumatology Workforce Gap with a Spotlight on Medicine-pediatrics Residency Trained Rheumatologist Career Paths [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/few-and-far-between-addressing-the-pediatric-rheumatology-workforce-gap-with-a-spotlight-on-medicine-pediatrics-residency-trained-rheumatologist-career-paths/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/few-and-far-between-addressing-the-pediatric-rheumatology-workforce-gap-with-a-spotlight-on-medicine-pediatrics-residency-trained-rheumatologist-career-paths/