Session Information
Date: Tuesday, November 9, 2021
Title: Systemic Sclerosis & Related Disorders – Clinical Poster III (1836–1861)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Esophageal dysmotility is a common feature of systemic sclerosis (SSc) and aspiration of gastric contents may serve as an inciting and/or exacerbating factor in the pathogenesis of interstitial lung disease (ILD). The present study aimed to: (1) determine whether the severity of gastroesophageal reflux predicts progression of SSc-ILD and (2) evaluate whether proton pump inhibitors (PPI) moderate the relationship between reflux severity and ILD progression as defined both radiographically and physiologically.
Methods: The UCLA SCTC GIT 2.0 was used to assess the severity of reflux in participants of Scleroderma Lung Study (SLS) II (Tashkin et al. Lancet Resp Med 2016). SLS II compared 24 months of mycophenolate versus 12 months cyclophosphamide followed by 12 months of placebo in patients with active SSc-ILD. A multivariable linear regression analysis was used to evaluate the relationship between baseline reflux scores and change in quantitative extent of radiographic ILD (QILD) and fibrosis (QLF) in the whole lung at 24 months. A joint model was created to evaluate the relationship between baseline reflux scores and the course of the forced vital capacity (FVC)%-predicted measured every 3 months over 24 months. All models controlled for treatment arm and baseline ILD severity, and tested whether PPI use was associated with ILD progression.
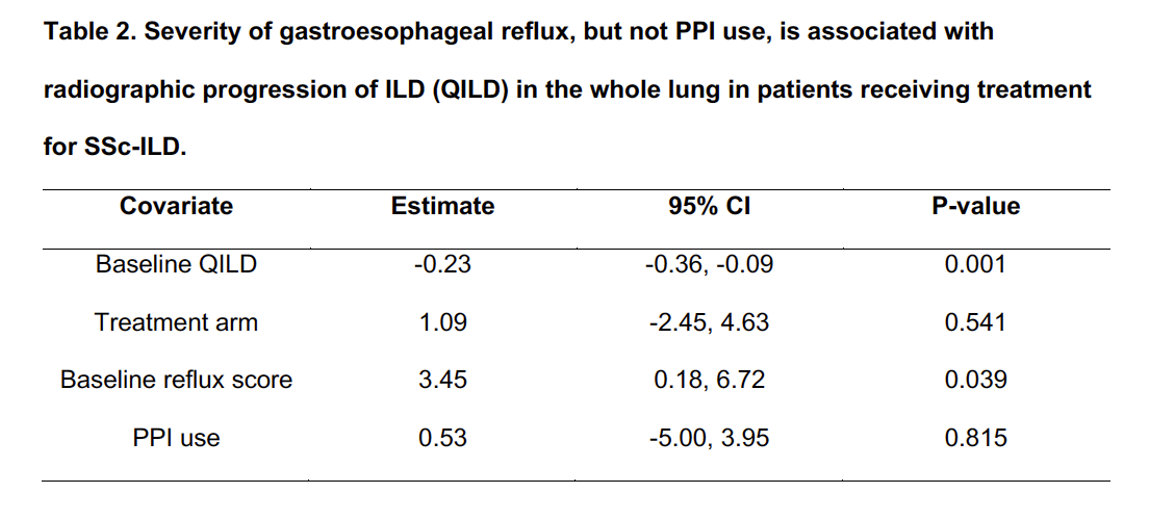
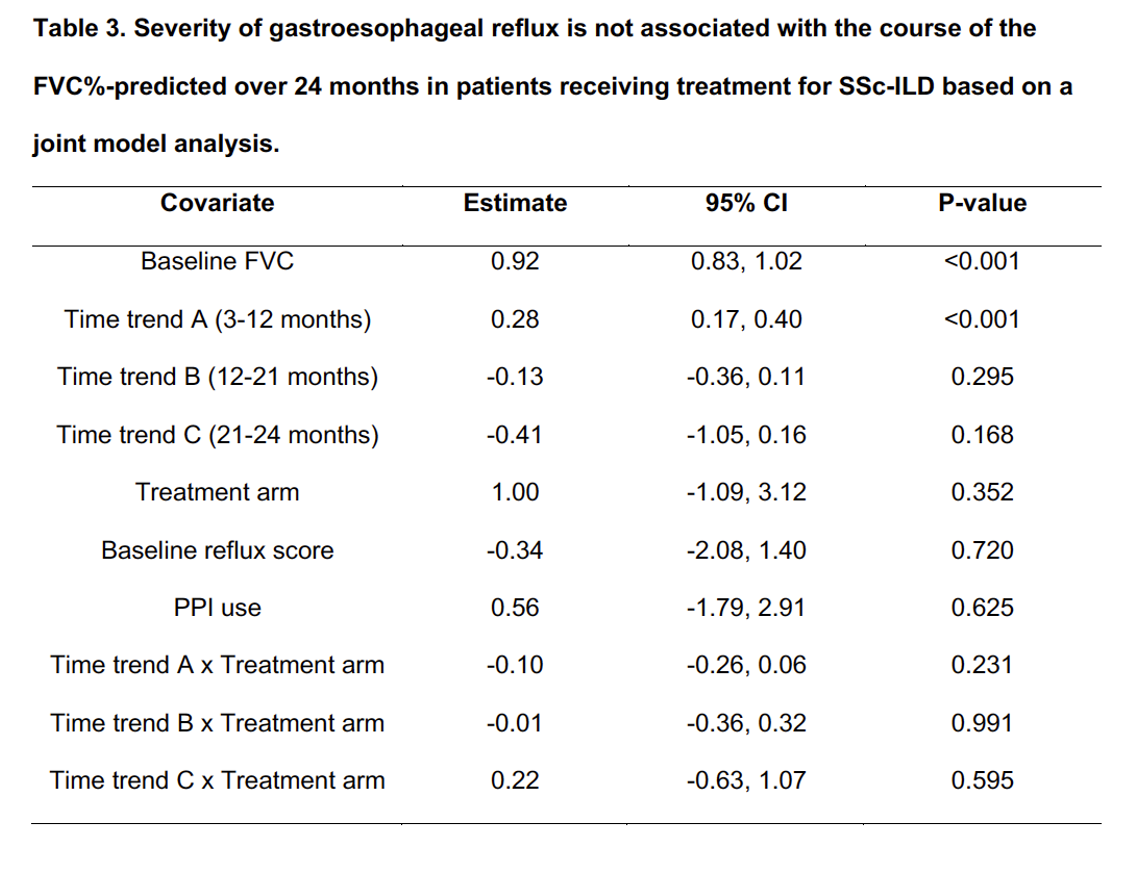
Results: 141 of the 142 SLS II participants had reflux scores at baseline and the mean score was 0.57, indicating moderate severity. There were no significant correlations between baseline reflux score and FVC%-predicted, QLF, QILD, disease duration, skin score, gender or the presence of diffuse cutaneous disease. Among participants with follow up HRCT scans (N=96), increased severity of reflux was significantly associated with increased QLF (Table 1) and QILD (Table 2) scores at 24 months. However, increased severity of reflux was not significantly associated with the course of the FVC%-predicted (N=130; Table 3). 112 (78.9%) of SLS II participants were taking a PPI at baseline; PPI users had higher reflux scores than non-users (P= < 0.0001). PPI use was not significantly associated with progression of ILD in any of the models.
Conclusion: Among patients receiving treatment for SSc-ILD, increased severity of gastroesophageal reflux symptoms was associated with ILD progression, based on worsening extent of radiographic fibrosis and total ILD, but not with the course of the FVC. PPI use was not associated with progression of ILD, suggesting that aspiration of non-acid gastric contents may play a role in perpetuating inflammation and fibrosis in SSc-ILD. Future studies are needed to assess whether other reflux treatments (e.g., pro-motility agents) moderate the relationship between reflux severity and ILD progression in SSc.
To cite this abstract in AMA style:
Volkmann E, Tashkin D, Leng M, Kim G, Goldin J, Roth M. Severity of Gastroesophageal Reflux, but Not the Use of Proton Pump Inhibitors, Is Associated with Radiographic Progression of Interstitial Lung Disease in Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/severity-of-gastroesophageal-reflux-but-not-the-use-of-proton-pump-inhibitors-is-associated-with-radiographic-progression-of-interstitial-lung-disease-in-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/severity-of-gastroesophageal-reflux-but-not-the-use-of-proton-pump-inhibitors-is-associated-with-radiographic-progression-of-interstitial-lung-disease-in-systemic-sclerosis/