Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: A large proportion of individuals with rheumatoid arthritis (RA), between 45%-70%, report sleep problems. Despite frequent reports of sleep problems, however, studies using objective measures of sleep in RA are rare, but are needed to provide greater accuracy than classifications based on self-report. Sleep disturbances may have unique causes and consequences in RA related to disruptions in the circadian rhythms of inflammatory and neuroendocrine biomarkers. We report objectively measured sleep characteristics among a cohort of individuals with RA and the associations with self-reported and physician-assessed disease activity.
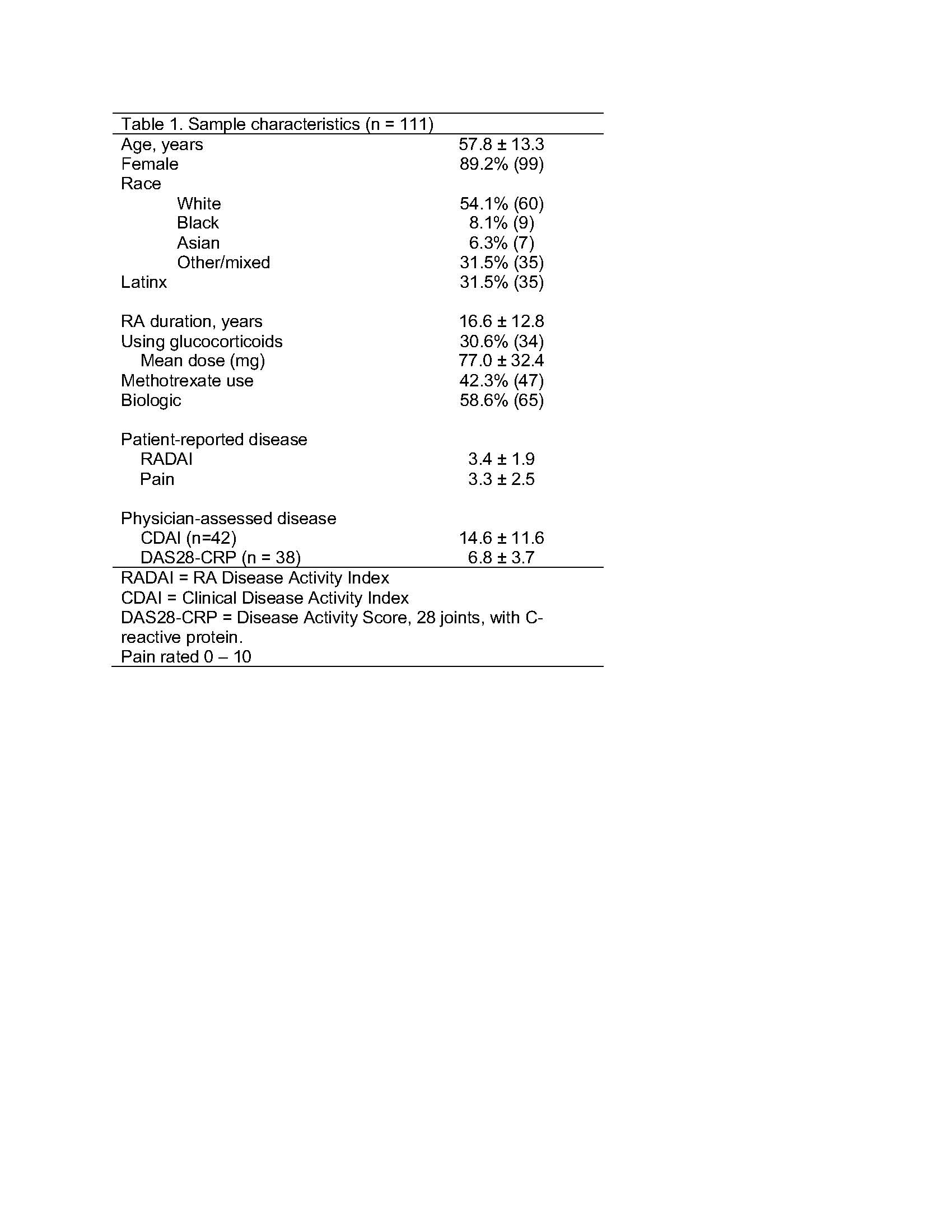
Methods: Data are from the baseline assessment of an ongoing longitudinal study of sleep disturbances in RA, in which 111 participants completed at least 4 nights of sleep monitoring using an Actigraph GT9X. The following sleep parameters were examined and compared to age and sex reference values from polysomnography: total sleep time, sleep efficiency (minutes sleeping/minutes in bed), number of awakenings/night (measure of fragmented sleep), and duration of awakenings/night (WASO [wake after sleep onset], also a measure of fragmented sleep). Total time in bed was also examined. The RA Disease Activity Index (RADAI) was used as a patient-reported measure of disease activity. RADAI includes self-reports of pain, painful joint counts, morning stiffness time, and patient global assessments. Physician-assessed disease activity using the Clinical Disease Activity Index (CDAI) and the Disease Activity Score-28 joints (DAS28-CRP) was available for a subset of participants who had in-person research visits prior to the onset of the pandemic. Analyses tabulated the frequency of poor sleep based on reference values and used t-tests to examine differences in RADAI, CDAI, and DAS28-CRP between those with poor vs. normal sleep.
Results: Participant characteristics are shown in Table 1. Sleep characteristics are shown in Table 2. Compared to age and sex references, 57.9% had short sleep time, 74.4% had poor sleep efficiency, 87.4% had high WASO, and 19.8% had a high number of awakenings. Poor sleep efficiency was associated with significantly worse patient-reported disease activity (Table 3). There were no significant associations between other sleep parameters and patient-reported disease activity. Short sleep time, a high number of nighttime awakenings, and long time in bed were each associated with significantly worse physician-assessed disease activity (Table 3). There were no significant associations between sleep efficiency or WASO and physician-assess disease activity.
Conclusion: In this sample of individuals with RA, a high proportion exhibited sleep disturbances compared to age and sex reference groups, and sleep disturbances were associated with both patient-reported and physician-assessed disease activity. It will be important in future studies to examine the causal directions of the relationships between poor sleep and disease activity.
To cite this abstract in AMA style:
Katz P, Patterson S, Nakamura M, Prather A, Trupin L, Rush S, Stone K. Association of Objectively Measured Sleep Characteristics with Rheumatoid Arthritis Disease Activity [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/association-of-objectively-measured-sleep-characteristics-with-rheumatoid-arthritis-disease-activity/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-objectively-measured-sleep-characteristics-with-rheumatoid-arthritis-disease-activity/