Session Information
Date: Tuesday, November 9, 2021
Title: Patient Outcomes, Preferences, & Attitudes Poster IV: COVID-19 (1589–1613)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: The impact of the COVID-19 pandemic on the mental and physical well-being of patients with systemic rheumatic diseases (SRDs) remains to be quantified. We assembled a cohort of Rheumatology outpatients with history of COVID-19 and compared HRQOL in patients with and without SRD over the course of the pandemic.
Methods: Between April 24, 2020 and May 26, 2020 we emailed a secure web-based survey to 26,045 patients ≥age 18 evaluated by a rheumatologist at a specialty hospital in New York City. A follow-up survey was sent in March 2021.SRD and non-SRD patients had relevant ICD-10-CM codes on ≥ 2 visits at least 7 days apart. Patients with an SRD code at only 1 visit were excluded. Non-SRD patients also had no SRD ICD-10-CM code. In this analysis, we included patients diagnosed with COVID-19 by a positive SARS-CoV-2 PCR or antigen test, or who were told by a medical provider they likely had COVID-19. The latter was included because in early 2020 SARS-CoV-2 tests were not readily available. Patients self-reported demographics on the first survey, and select PROMIS-29 domains at both time points. We used paired T-tests to compare within person change, and T-tests and Chi-Square to compare differences between groups.
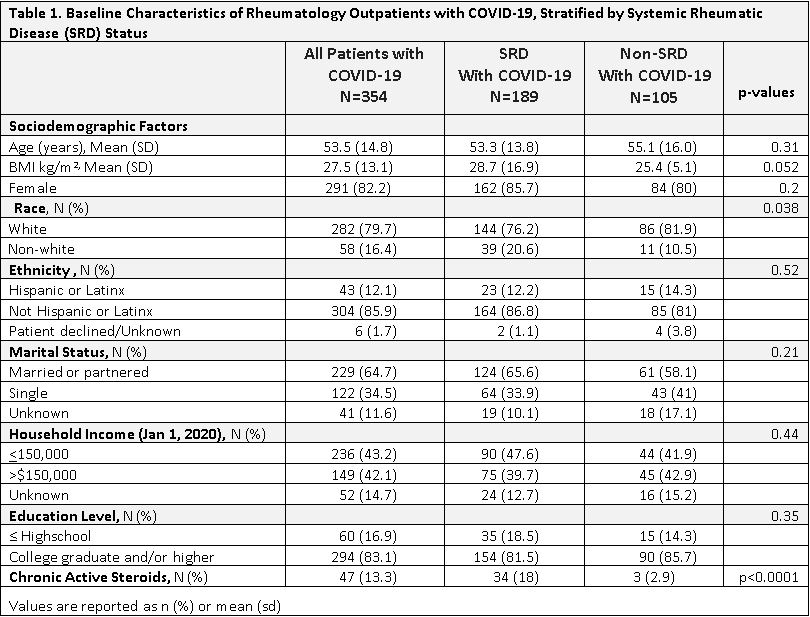
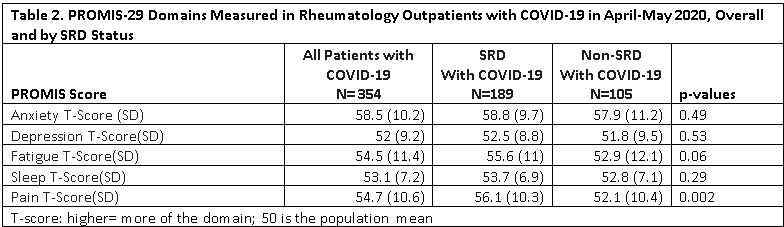
Results: Of 6584 (25.3%) patients responding to the PROMIS-29 on the first survey, 354 subjects reported having COVID-19; of those 189 met SRD and 105 met non-SRD criteria. SRD and non-SRD patients were of similar age (53.3 vs. 55.1 years), percent female (85.7% vs 80%), and body mass index (28.7 vs. 25.4). Patients with SRD were more likely to be White (76.2% vs. 81.9%; p=0.038) and be on chronic active corticosteroids (18% vs 2.9%; p< 0.0001). Overall, 17.5% went to an emergency room, though few were hospitalized (6.9% SRD vs. 4.8% non-SRD, p=0.47) . At baseline, SRD and non-SRD patients had similar PROMIS-29 T-scores except SRD had worse pain (Table 1). Of 100 subjects reporting PROMIS-29 at both time points, within-person changes for the fatigue domain indicated worsening only in SRD (T-score difference of 4.6; p= 0.02). 44% of SRD subjects compared with only 28% of non-SRD subjects reported clinically meaningful (T-score >=5) worse fatigue at follow up; p< 0.028). There was no significant association between clinically meaningfully worse fatigue at follow up and use of chronic active corticosteroids, going to the ER, or being hospitalized (data not shown).
Conclusion: Although all subjects with a history of COVID-19 had similar PROMIS-29 scores at baseline, subjects with SRD were 1.6 x more likely to report clinically meaningful worsening of fatigue nearly 1 year after COVID-19 diagnosis, compared to non-SRD patients followed at the same Rheumatology practice. Analysis is ongoing to identify predictors of poor HRQOL after COVD-19 in patients with SRD.
To cite this abstract in AMA style:
Mandl L, Levine J, Bykerk V, Barbhaiya M. Health Related Quality of Life in Rheumatology Outpatients with COVID-19 from New York City over the Course of the Pandemic [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/health-related-quality-of-life-in-rheumatology-outpatients-with-covid-19-from-new-york-city-over-the-course-of-the-pandemic/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/health-related-quality-of-life-in-rheumatology-outpatients-with-covid-19-from-new-york-city-over-the-course-of-the-pandemic/