Session Information
Date: Monday, November 8, 2021
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Frailty, a syndrome characterized by decreased physiologic reserve, is associated with chronic inflammation. We have shown a high prevalence of frailty in patients with polymyalgia rheumatica (PMR) using the Fried criteria (FC), the gold standard frailty phenotypic instrument1. However, the FC is not practical to use at point of care. The Frail scale (FS), an easy-to-use self-report frailty instrument, has not been evaluated in patients with PMR. The objectives of this study were to evaluate the prevalence of frailty using the FS, to compare its performance with the FC, and to describe the association of frailty with health-related quality of life (HRQoL) in patients with PMR.
Methods: Patients with PMR who fulfilled 2012 EULAR/ACR Provisional Classification Criteria at time of diagnosis, ≤ 12 months from diagnosis and on active treatment with glucocorticoids were recruited from a single center. Disease activity was measured with the PMR-activity score. Comorbidity burden was measured by the Charlson Comorbidity Index (CCI). Frailty and pre-frailty were defined according to FC and the FS2. HRQoL was assessed using global Patient-Reported Outcomes Measurement Information System (PROMIS) computerized adaptive tests. Sarcopenia was assessed by DXA. Fisher’s exact test, chi-square tests and Kruskal-Wallis tests were used to describe differences among groups as appropriate. Frailty according to FC and FS were compared using a Spearman correlation.
Results: 41 patients completed a baseline visit. 12% and 17% of patients were frail, and 54% and 59% were pre-frail according to the FS and FC, respectively (Table 1). There was a strong correlation between the FRAIL scale and the Fried frailty criteria (r = 0.71, p < 0.05). Based on the FS, there were significant differences in the sex and CCI among frail, pre-frail, and robust patients (p = 0.03) (Table 2). Although non-significant, frail patients had higher CRP at diagnosis and ESR at study visit. According to both definitions, frail patients had more pain behavior (FS: p=0.04; FC: p=0.01) and pain interference (FS: p=0.02; FC: p< 0.01) (Table 3). Additionally, according to FS, frail patients also had more fatigue (p=0.02) and anxiety (p=0.02), and worse physical function (p=0.01). Pre-frail patients, according to FS, had more sarcopenia (p=0.02). There were no differences in disability according to either definition.
Conclusion: There was a higher prevalence of frailty and pre-frailty in this cohort of patients with PMR. Despite similar disease duration, comorbidity burden, and dose of glucocorticoids, frail patients with PMR had statistically significant and clinically meaningful worse HRQoL. There was a strong correlation between self-reported frailty and a standard frailty measure suggesting the use of the FS as a simple frailty screening tool for patients with PMR in clinical practice.
References:
< !1. Sattui SE, et al. Arthritis Rheumatol. 2020; 72 (suppl 10).
< !2. Morley JE et al. J Nutr Health Aging 2012;16:601.
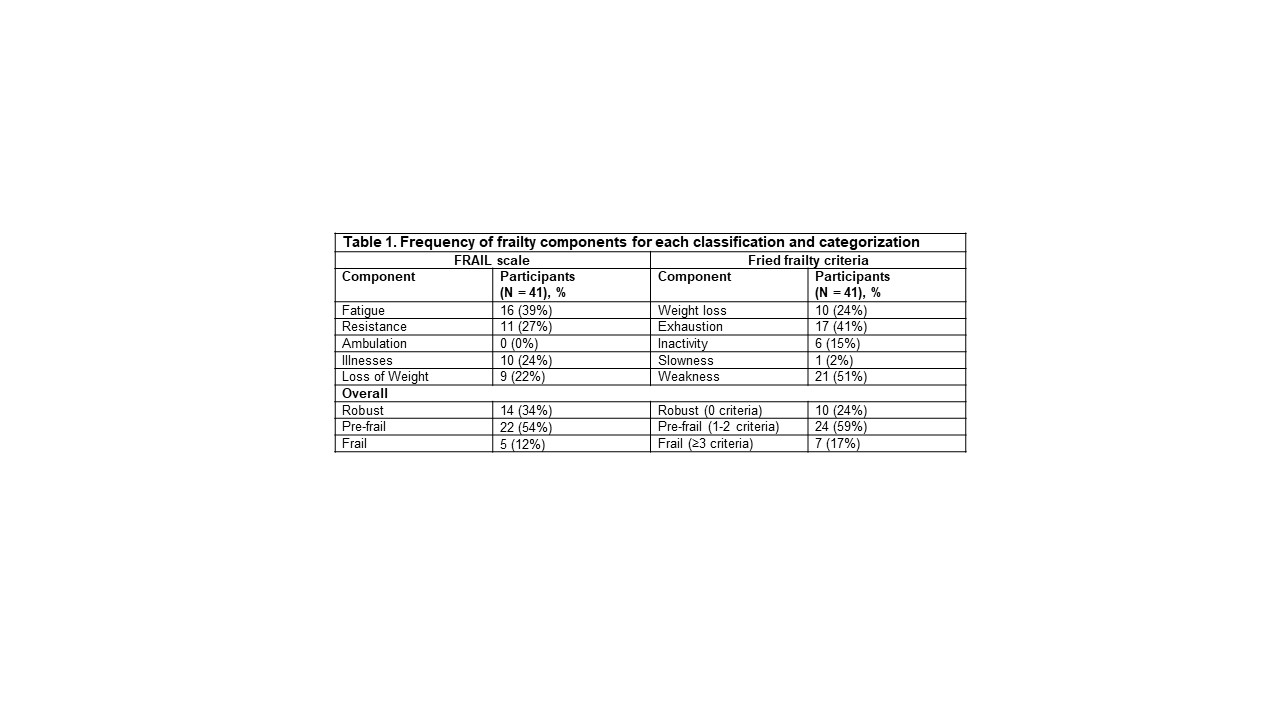 Table 1. Frequency of frailty components for each classification and categorization
Table 1. Frequency of frailty components for each classification and categorization
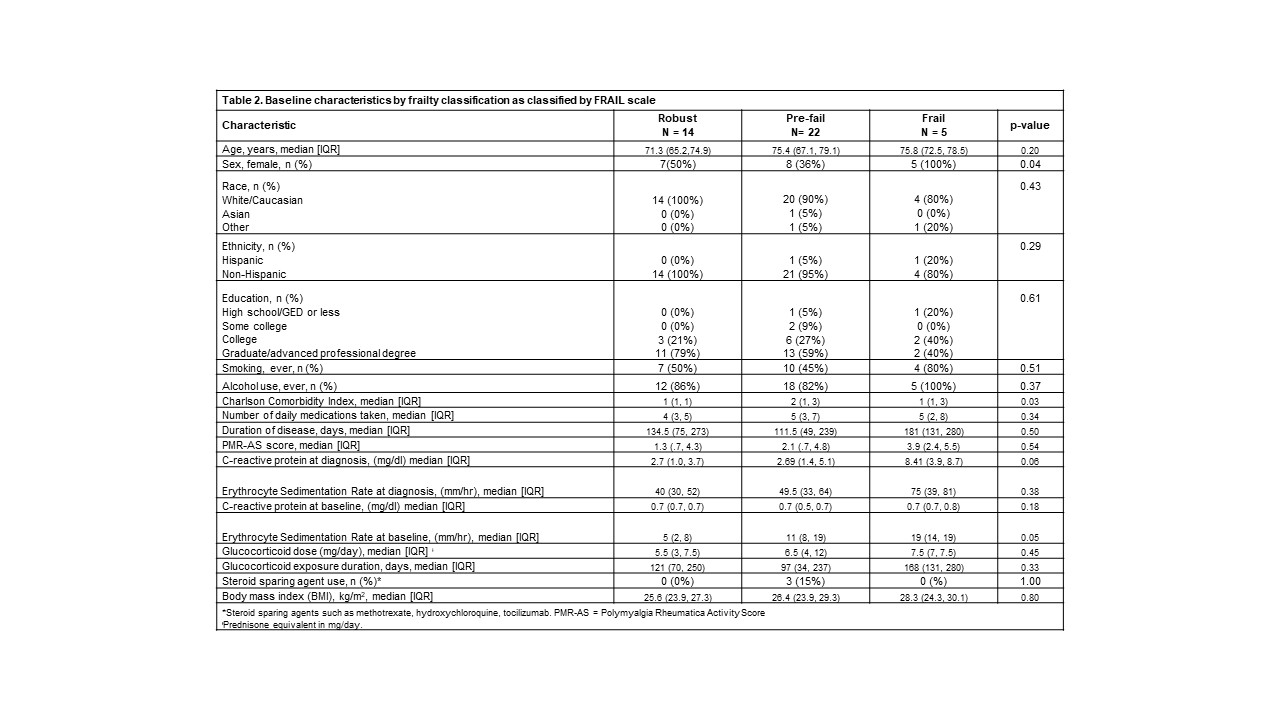 Table 2. Baseline characteristics by frailty classification as classified by FRAIL scale
Table 2. Baseline characteristics by frailty classification as classified by FRAIL scale
 Table 3. Health-related Quality of Life, Sarcopenia and Disability by frailty classification
Table 3. Health-related Quality of Life, Sarcopenia and Disability by frailty classification
To cite this abstract in AMA style:
Sattui S, Jannat-Khah D, Lally L, Lieber S, Mandl L, Spiera R. Assessment of a Patient Self-Report Frailty Tool in Patients with Polymyalgia Rheumatica [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/assessment-of-a-patient-self-report-frailty-tool-in-patients-with-polymyalgia-rheumatica/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessment-of-a-patient-self-report-frailty-tool-in-patients-with-polymyalgia-rheumatica/
