Session Information
Date: Monday, November 8, 2021
Title: Systemic Sclerosis & Related Disorders – Clinical Poster II (1364–1390)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Scleroderma is associated with underlying ILD. About 48% those with diffuse cutaneous SSc and 26% of those with limited cutaneous SSc were found to have ILD on HRCT based on prior literature. The most common cause of mortality in Scleroderma has shifted from renal crisis to pulmonary diagnoses. In our study, we aim to identify the risk factors and outcomes of acute respiratory failure in patients with underlying ILD and Scleroderma.
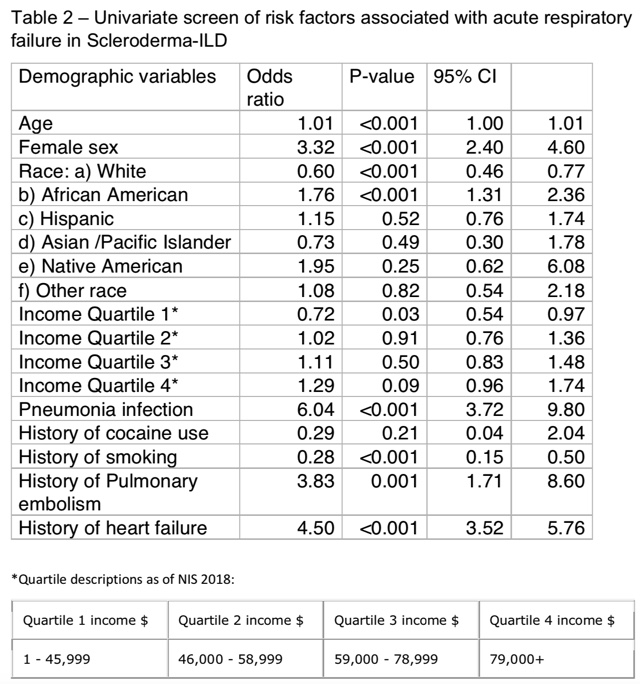
Methods: Data were abstracted from the National Inpatient Sample (NIS) Database. This database is the largest collection of inpatient admission data in the USA. It is a nationally representative sample of 20% of hospitalizations from approximately 1000 hospitals. The NIS was searched for hospitalizations in 2016, 2017 and 2018 containing ICD-10 for acute respiratory failure codes with J96 as principal diagnosis and underlying Scleroderma associated with ILD as secondary diagnoses with codes M34.81, J84 and J98.4. Using STATA software, the total number of discharges, age, race, length of stay (LOS), mortality and total hospital charges were recorded. A univariate logistic regression analysis was used to calculate unadjusted odds ratios (ORs) for a principal diagnosis of acute respiratory failure. All variables with p-values < 0.2 were included in a multivariate logistic regression model. P-values < 0.05 were considered significant in the multivariate analysis.
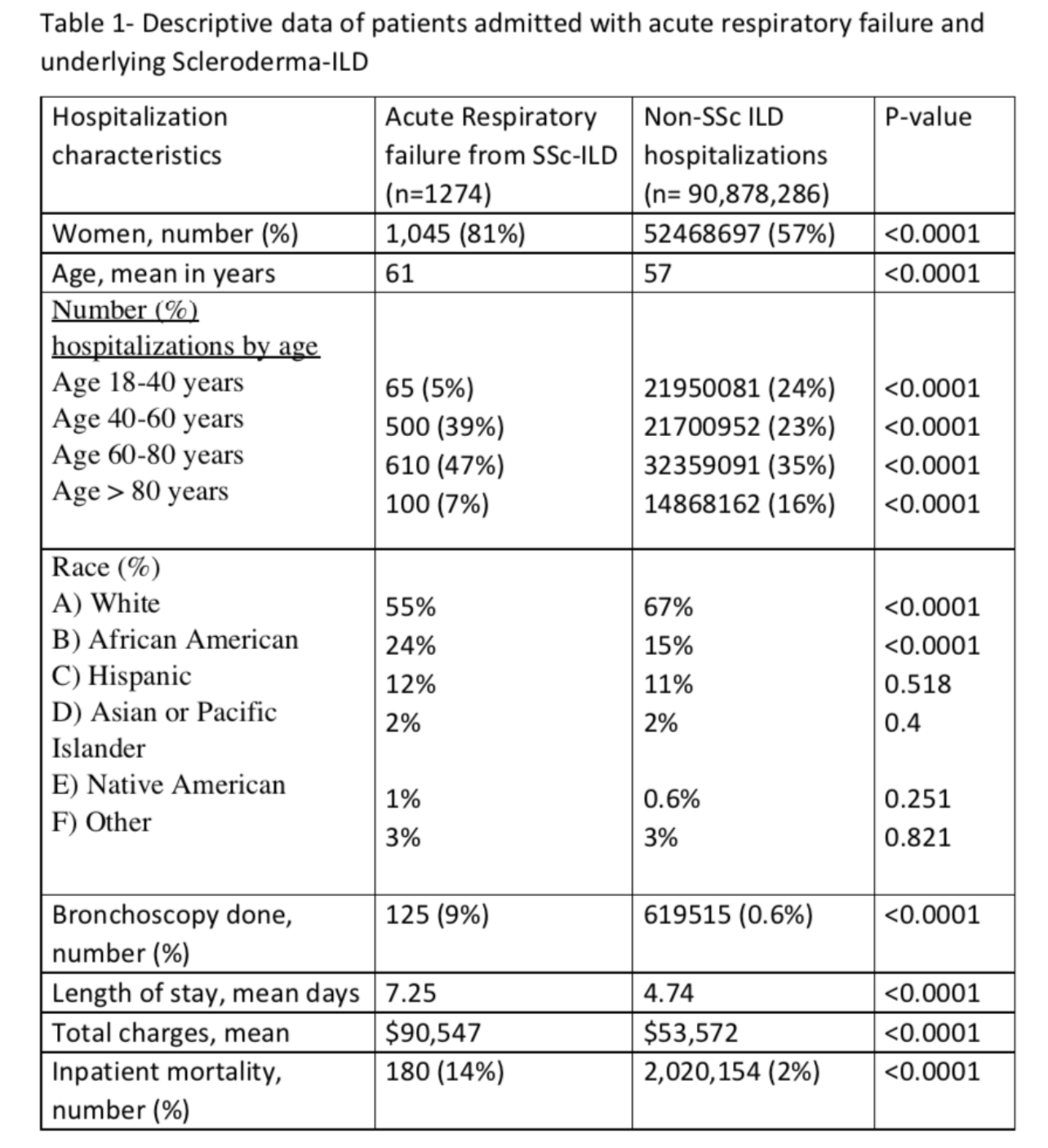
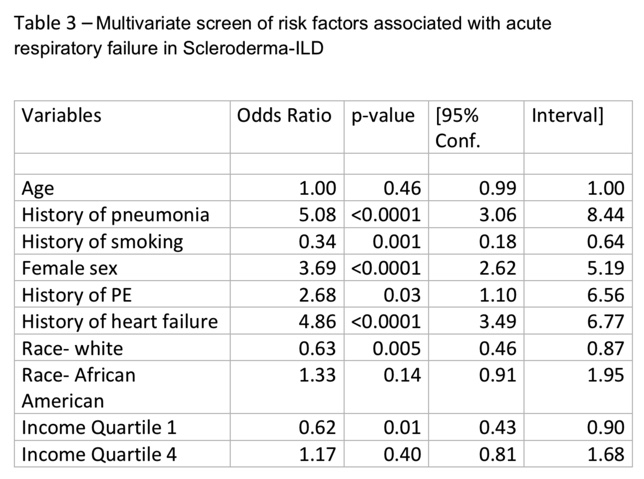
Results: A total number of 1,274 patients with underlying Scleroderma-ILD were hospitalized for acute respiratory failure in 2016, 2017 and 2018. Characteristics of patients with acute respiratory failure and underlying Scleroderma vs all other adult hospitalizations are displayed in table 1. When compared to the reference group, females were 81% vs 57%. Mean age was 61 yrs vs 57 yrs Caucasians formed 55% vs 67%, followed by African Americans 24% vs 15%. 125 (9%) patients underwent BAL vs 0.6%. Mean LOS was 7.25 days vs 4.74 days, mean total charge of hospitalization was $90,547 vs $53,572. Inpatient mortality was 14% vs 2%. The following were found to be significant risk factors for acute respiratory failure among scleroderma ILD patients in multivariate analysis: pneumonia OR 5.0, Heart failure OR 4.8, female sex OR 3.6, PE OR 2.6, white race OR 0.6, Quartile 1 of income status based on zip code OR 0.6 and smoking OR 0.3
Conclusion: This analysis represents the largest sample to-date to assess the incidence, mortality, and risk factors for development of acute respiratory failure among Scleroderma patients with ILD. Results show slightly higher mean age in this group compared to the reference group. The cost of hospitalization and inpatient mortality are also noted to be significantly higher. Female sex, pneumonia, PE, and heart failure are risk factors for acute respiratory failure. This study emphasizes that Scleroderma-ILD patients have high inpatient mortality. Prompt recognition of respiratory distress and pro-active management of above risk factors should be studied as means to improve inpatient scleroderma outcomes.
To cite this abstract in AMA style:
Kambhatla S, Manadan A, Trang A. Outcomes and Risk Factors for Respiratory Failure in Patients with Scleroderma Associated with ILD [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/outcomes-and-risk-factors-for-respiratory-failure-in-patients-with-scleroderma-associated-with-ild/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-and-risk-factors-for-respiratory-failure-in-patients-with-scleroderma-associated-with-ild/