Session Information
Date: Monday, November 8, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster III: Outcomes (1257–1303)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Lupus nephritis (LN) is a severe manifestation of systemic lupus erythematosus (SLE), occurring in approximately 40% of SLE patients (pts) and often resulting in the development of chronic kidney disease (CKD) and permanent kidney damage.1 CKD is categorized by progressive disease stages (1-5) based on kidney biopsy, ultimately resulting in end-stage kidney disease (Stage 5). While healthcare costs of CKD by stage for broad CKD populations have been quantified,2,3 few studies have examined CKD costs among SLE pts. This study described and compared disease severity and healthcare costs for SLE pts with and without CKD in the United States of America.
Methods: A retrospective analysis (GSK Study 217378) was conducted using claims data from the Optum Research Database. Adults who had ≥2 outpatient medical claims or ≥1 inpatient claim for SLE from January 1, 2018, to December 31, 2018 (identification period), were assessed. During the identification period, SLE pts with CKD were identified based on ≥1 CKD International Classification diagnosis code and were subsequently categorized based on their highest diagnosed CKD stage (date of highest CKD stage=index). SLE pts without CKD were required to have no CKD diagnoses (date of their first SLE diagnosis=index). Pts’ characteristics and disease severity were assessed for the baseline period (12 months pre index). Healthcare costs (in 2019 US$) were assessed for the observation period (January 1, 2019, to December 31, 2019) for SLE pts with CKD (overall and by CKD stage) and SLE pts without CKD.
Results: A total of 2666 SLE patients with CKD and 9488 SLE patients without CKD met study criteria. Patients were mostly female (CKD: 86.6%; no CKD: 91.1%) with a mean (standard deviation, SD) age of 63.9 (14.1) (CKD) and 57.8 (14.5) (no CKD) years. During the baseline period, SLE patients with CKD had greater disease activity than SLE patients without CKD (moderate-severe disease: 93.9% vs 66.4%; ≥1 flare of any severity: 96.5% vs 92.0%; mean [SD] number of flares: 5.9 [3.1] vs 4.7 [2.8]). Also, 4.1% of SLE patients with CKD had evidence of biopsy versus 0.2% of SLE patients without CKD, and 76.9% had LN versus 3.0% of SLE patients without CKD. During the observation period, mean (SD) annual healthcare costs were substantially higher for SLE patients with CKD versus those without CKD ($59,956 [100,785] vs $31,652 [57,781]). In addition, costs increased with advancing stages of CKD, from $36,417 ($56,028) (Stage 1) to $152,169 ($177,656) (Stage 5) (Figure).
Conclusion: SLE patients with CKD had more severe disease and incurred higher annual healthcare costs compared with SLE patients without CKD. Among SLE patients with CKD, healthcare costs increased with each CKD stage progression. These results demonstrate the substantial burden of CKD in patients with SLE and highlight the need to manage SLE to prevent progression to CKD.
References:
1Hanly J, et al. Rheumatology 2016;55(2):252–62
2Honeycutt AA, et al. J Am Soc Nephrol 2013;24(9):1478–83
3Golestaneh L, et al. Am J Managed Care 2017;23:S163–72
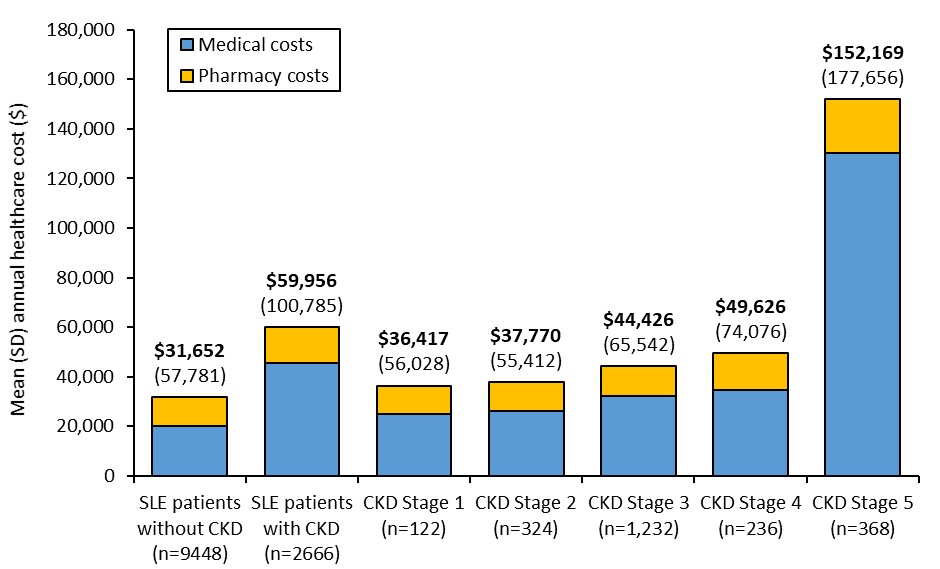 Annual healthcare cost per patient among SLE patients with and without CKD
Annual healthcare cost per patient among SLE patients with and without CKD
To cite this abstract in AMA style:
Huang S, Guisinger A, Averell C, Bell C. Disease Severity and Healthcare Costs Associated with Chronic Kidney Disease in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/disease-severity-and-healthcare-costs-associated-with-chronic-kidney-disease-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/disease-severity-and-healthcare-costs-associated-with-chronic-kidney-disease-in-patients-with-systemic-lupus-erythematosus/
