Session Information
Session Type: Abstract Session
Session Time: 10:30AM-10:45AM
Background/Purpose: Although several studies indicate that patients with COVID-19 produce antiphospholipid antibodies (aPL), it is unclear which aPL subtype predominates and whether aPL correlates with thrombosis or severe COVID-19 outcomes. We tested aPL in a large prospective cohort of patients with and without COVID-19, and determined if aPL are associated with thromboembolic events and other severe outcomes in hospitalized COVID-19 patients.
Methods: Symptomatic patients undergoing SARS-CoV-2 nasopharyngeal PCR testing at a Canadian tertiary centre were enrolled in a prospective biobank cohort from March-July 2020. All PCR results (including those performed at other centres), demographics, medical history, hospitalization details and clinical outcomes were collected with a standard report form. Subjects were classified as COVID+ (≥1 positive PCR prior/at baseline) or non-COVID (all PCR negative prior/after enrolment). Biobanked plasma (day 0-7 after enrolment) was tested for anticardiolipin (aCL) IgM and IgG, anti-domain I of ß2-glycoprotein I (aD1ß2GP1) IgM and IgG, anti-phosphatidylserine/prothrombin (aPS/PT) IgM and IgG (Inova Diagnostics, San Diego), as well as lupus anticoagulant (LAC; Precision BioLogic, Halifax) using manufacturers’ cut-offs. All plasma was also tested for SARS-CoV-2 IgM and IgG. We compared aPL prevalence (including subtypes) between COVID+ and non-COVID subjects. In hospitalized COVID+ subjects, we performed multivariate logistic regressions evaluating aPL (and subtypes) and thrombotic events (deep vein thrombosis, DVT, pulmonary embolism, PE, stroke, transient ischemic attack, TIA, myocardial infarction, MI), as well as acute kidney injury (AKI), intensive care unit (ICU) stay, mechanical ventilation, and death, adjusting for age and sex.
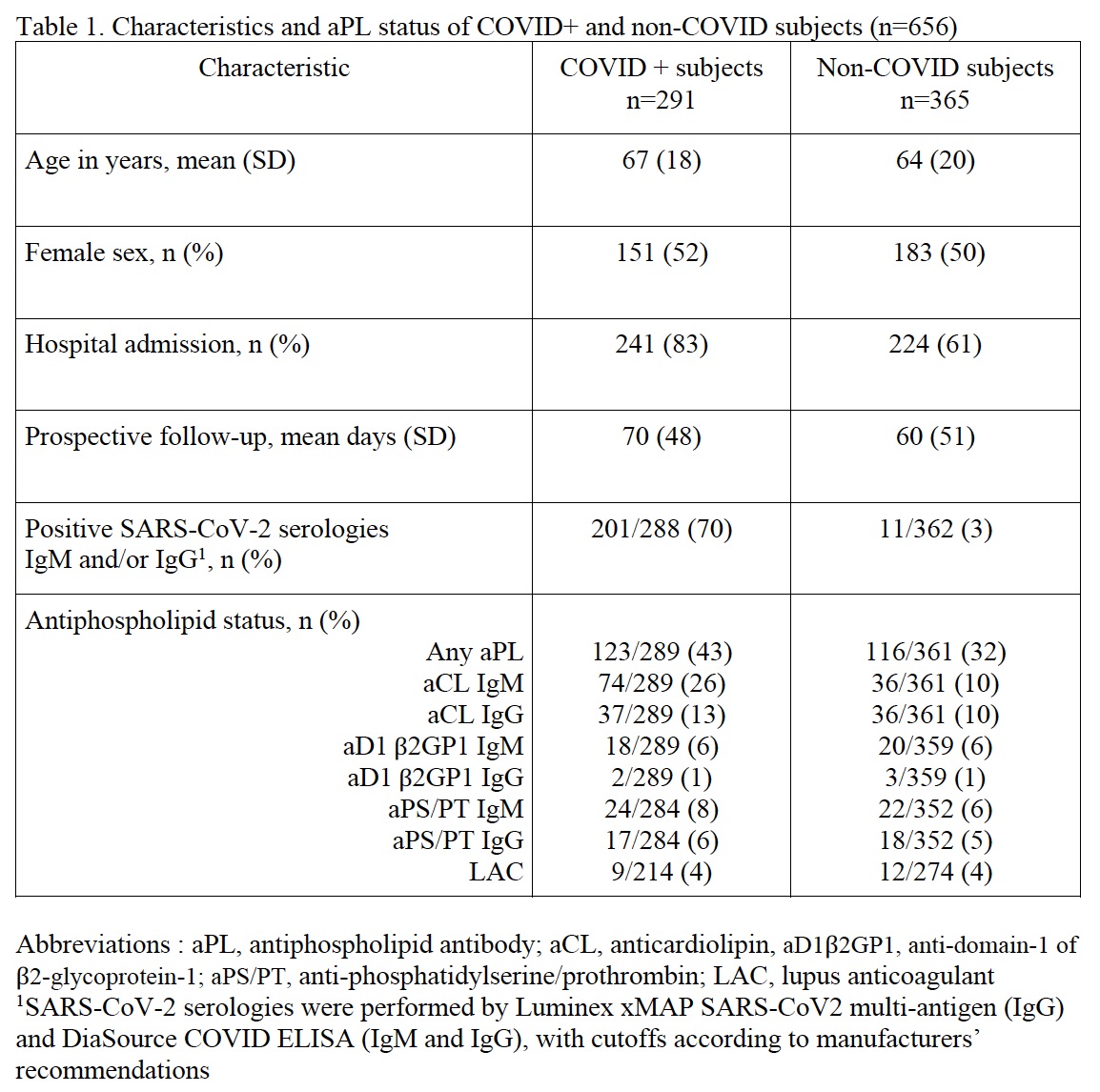
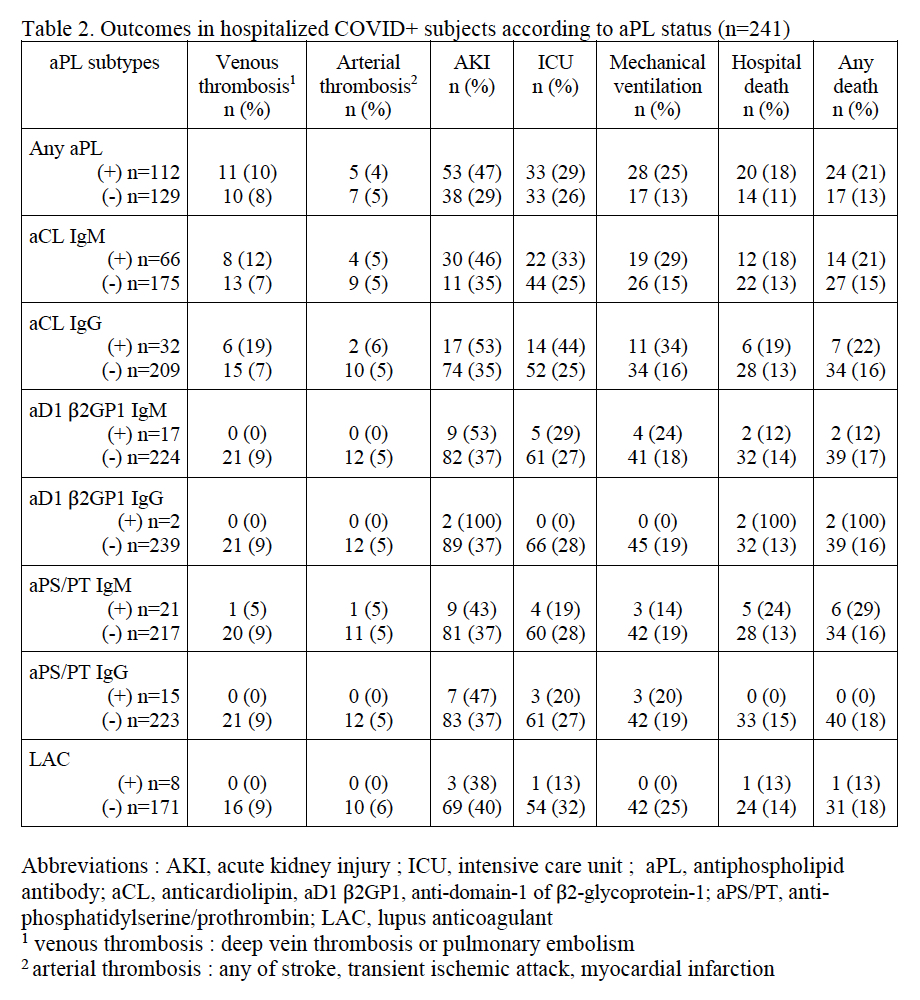
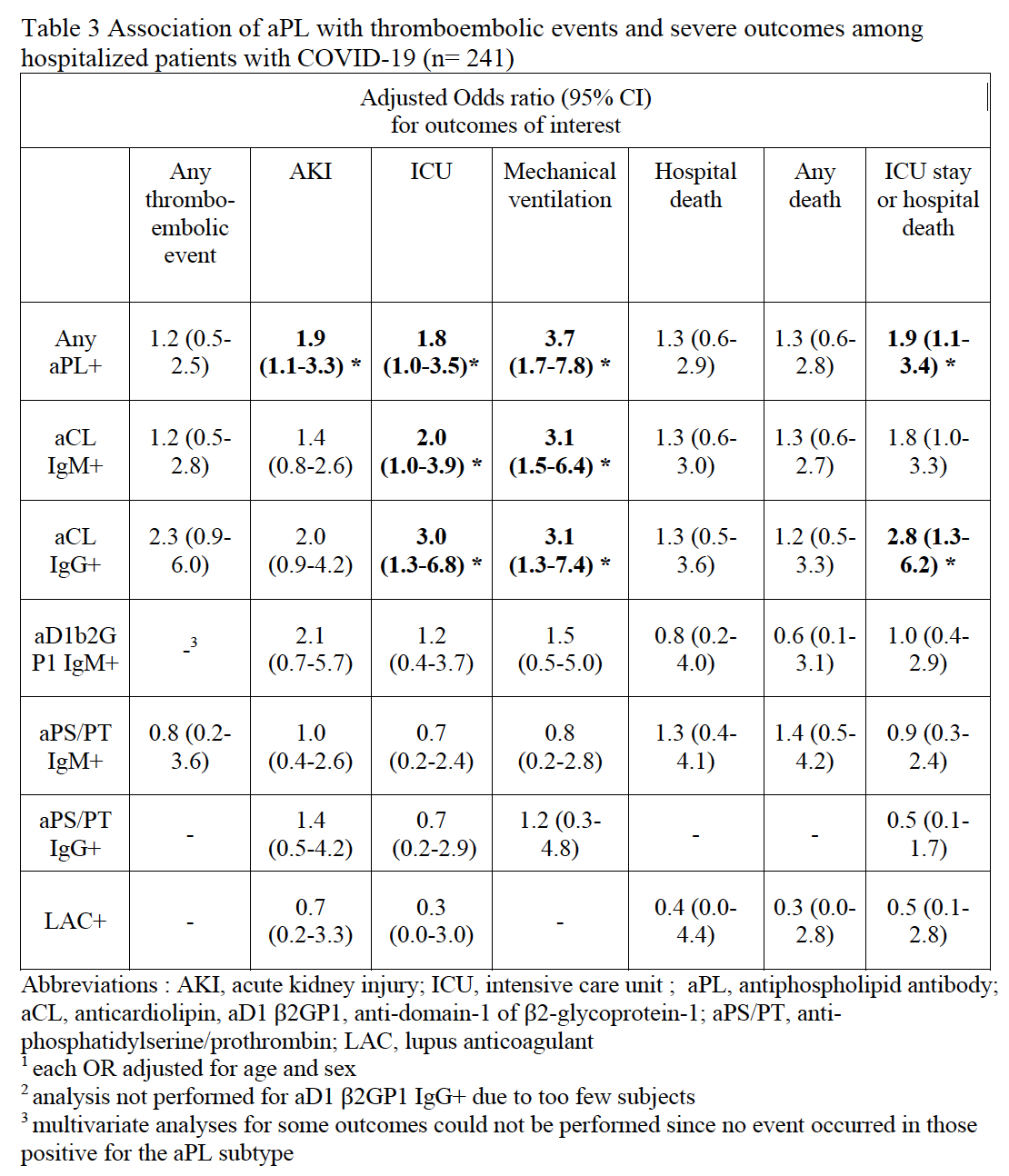
Results: We studied 291 COVID+ and 365 non-COVID patients. The two groups were similar in age and sex, but more COVID+ patients were hospitalized (83% vs 61%) and had positive SARS-CoV-2 serology (70% vs 3%) vs non-COVID patients (Table 1). At baseline, 43% of COVID+ patients were positive for at least one aPL versus 32% of non-COVID patients (difference in proportion 11%; 95% CI 3, 18). In hospitalized COVID+ patients, 13% had a thromboembolic event, 38% developed AKI, 27% had an ICU stay, 19% had mechanical ventilation, and 17% died. In multivariate analyses, presence of any aPL was associated with AKI (OR 1.9; 95% CI 1.1, 3.3), ICU stay (OR 1.8; 95% CI 1.0, 3.5) and mechanical ventilation (OR 3.7; 95% CI 1.7, 7.8). Both aCL IgM and aCL IgG were strongly and independently associated with ICU stay and mechanical ventilation (Table 3). We saw a strong trend for more thrombotic events associated with aCL IgG (OR 2.3; 95% CI 0.9, 6.0), though the CI included the null value.
Conclusion: In this large prospective sample, over 40% of COVID-19 patients had aPL early in their clinical course. In hospitalized COVID-19 patients, aPL were associated with substantial increased risk of severe outcomes, with a strong trend for association between aCL IgG and thrombotic events. Our findings suggest that aPL, in particular aCL, might be useful markers for risk stratification in COVID-19.
To cite this abstract in AMA style:
Mendel A, Fritzler M, St.Pierre Y, Rauch J, Bernatsky S, Vinet E. Association of Antiphospholipid Antibodies with Thromboembolic Events and Severe Outcomes in COVID-19 [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/association-of-antiphospholipid-antibodies-with-thromboembolic-events-and-severe-outcomes-in-covid-19/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-antiphospholipid-antibodies-with-thromboembolic-events-and-severe-outcomes-in-covid-19/