Session Information
Session Type: Abstract Session
Session Time: 9:00AM-9:15AM
Background/Purpose: Patients with primary systemic vasculitis (PSV) and polymyalgia rheumatica (PMR) may be at high risk for poor COVID-19 outcomes due to the treatments used, the potential organ damage caused by PSV, and demographic factors such as older age that are associated with these conditions. We investigated factors associated with COVID-19 outcomes in patients with PSV and PMR in a large multinational registry.
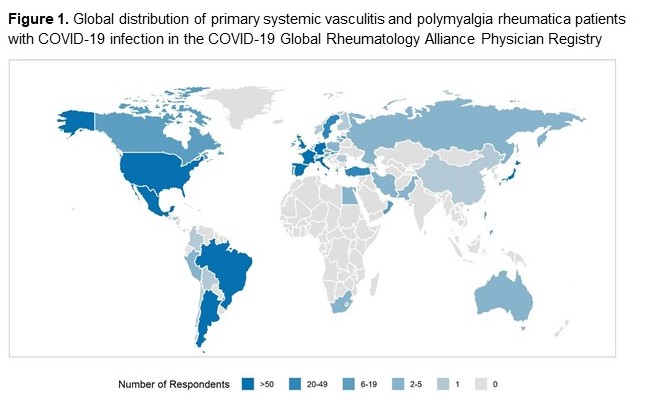
Methods: We analyzed PSV and PMR cases from the COVID-19 Global Rheumatology Alliance registries (12/Mar/2020-12/Apr/2021). PSV diagnoses included ANCA vasculitis (AAV), giant cell arteritis (GCA), Behçet’s syndrome, and other vasculitides. The ordinal COVID-19 severity outcome was: 1) no hospitalization, 2) hospitalization without oxygen, 3) hospitalization with oxygen/ventilation, or 4) death. Relevant covariates included age, sex, race, season, number of comorbidities, BMI, smoking status, disease activity, immunosuppresive therapies (conventional synthetic and biologic/targeted synthetic DMARDs), glucocorticoid (GC) (daily dose prednisolone-equivalent), and region. Multivariable ordinal logistic regressions were used to estimate odds ratios (ORs) for being one level higher on the ordinal outcome. Analyses were also stratified by disease (GCA, AAV, or PMR).
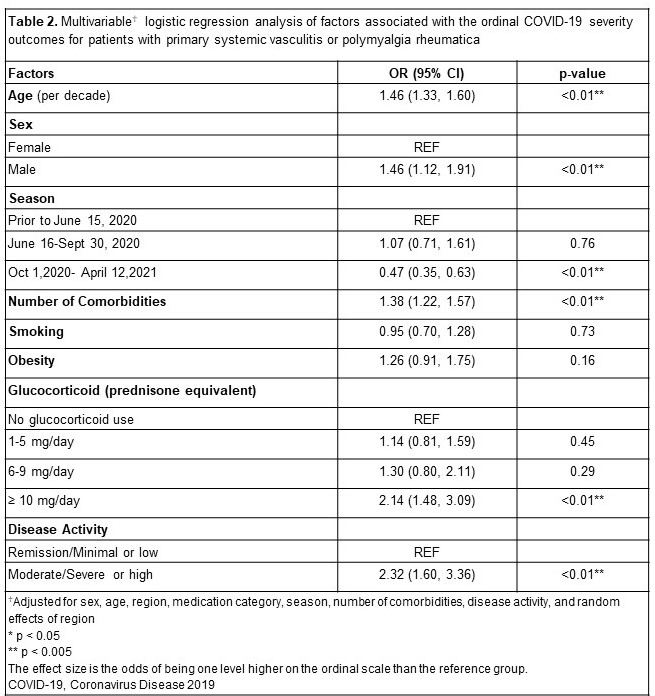
Results: Of 1,202 included patients, 61.0% were female; mean age was 63.8 years. Diagnoses were PMR (31.1%), AAV (29.3%), GCA (15.2%), Behçet’s syndrome (9.4%), and other vasculitis (15.0%). Overall, 508 (49.8%) patients were hospitalized, and 155 (15.2%) patients died (Table 1). Older age (OR 1.46, 95% CI 1.33-1.60), male sex (OR 1.46, 95% CI 1.12-1.91), GC dose ≥ 10 mg/day (OR 2.14, 95% CI 1.48-3.09), moderate/severe or high disease activity (OR 2.32, 95% CI 1.60-3.36) and number of comorbidities (OR 1.38, 95% CI 1.22-1.57) were associated with worse outcome (Table 2). In the disease-specific stratified analysis, 20.3% and 22.2% of patients with GCA and AAV, respectively, died. Risk factors for poorer outcomes were: for GCA patients, older age (OR 1.79, 95% CI 1.21-2.65) and obesity (OR 3.04, 95% CI 1.17-3.04); for AAV patients, older age (OR 1.45, 95% CI 1.18-1.79), rituximab (OR 2.50, 95% CI 1.33-4.68) or cyclophosphamide use (OR 6.43, 95% CI 1.48-28.01), and moderate/severe or high disease activity (OR 2.71, 95% CI 1.21-6.07); and for polymyalgia rheumatica, older age (OR 2.69, 95% CI 1.99-3.63) and higher comorbidity burden (OR 1.31, 95% CI 1.03-1.67). Overall, severe outcomes were less likely if COVID-19 infection developed between October 1, 2020, and April 12, 2021 (OR 0.47, 95% CI 0.35-0.63). This was also observed in the disease-specific analysis.
Conclusion: Patients with GCA or AAV who had COVID-19 infection had higher rates of severe outcomes compared to PMR and other vasculitis, even despite similar ages of the GCA and PMR groups. Risk factors identified for different PSV subtypes may inform mitigation strategies for these patients.
To cite this abstract in AMA style:
Sattui S, Conway R, Putman M, Seet A, Beins K, Hill C, Liew D, Mackie S, Mehta P, Neill L, Gomez G, Salinas M, Maldonado F, Moriz H, Studart S, ARAUJO N, Knight A, Rozza D, Quartuccio L, Samson M, Bally S, Maria A, Chazerain P, Hasseli R, Müller-Ladner U, Hoyer B, Voll R, Torres R, Luis M, Ribeiro S, Al Emadi S, Sparks J, Hsu T, D'Silva K, Patel N, Wise L, Gilbert E, Valenzuela-Almada M, Duarte-Garcia A, Ugarte-Gil M, Sirotich E, Liew J, Hausmann J, Sufka P, Bhana S, Grainger R, Costello W, Jacobsohn L, Izadi Z, Strangfeld A, Frazão Mateus E, Hyrich K, Gossec L, Carmona L, Lawson-Tovey S, Kearsley-Fleet L, Schaefer M, Gianfrancesco M, Machado P, Wallace Z, Yazdany J, Robinson P. Outcomes of COVID-19 Infection in Patients with Primary Systemic Vasculitis and Polymyalgia Rheumatica: Results from the COVID-19 Global Rheumatology Alliance Physician Registry [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/outcomes-of-covid-19-infection-in-patients-with-primary-systemic-vasculitis-and-polymyalgia-rheumatica-results-from-the-covid-19-global-rheumatology-alliance-physician-registry/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-of-covid-19-infection-in-patients-with-primary-systemic-vasculitis-and-polymyalgia-rheumatica-results-from-the-covid-19-global-rheumatology-alliance-physician-registry/