Session Information
Date: Sunday, November 7, 2021
Title: Patient Outcomes, Preferences, & Attitudes Poster II: Measurements (0739–0763)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Fewer than 50% of patients with rheumatoid arthritis (RA) are treated using a TTT strategy. The purpose of this study was to better understand rheumatologists’ and patients’ decision making regarding TTT using the Mental Models Approach to Risk Communication (MMARC). The MMARC provides a rigorous framework to develop interventions that address critical discrepancies between the mental models held by different populations, in this context, rheumatologists and patients.
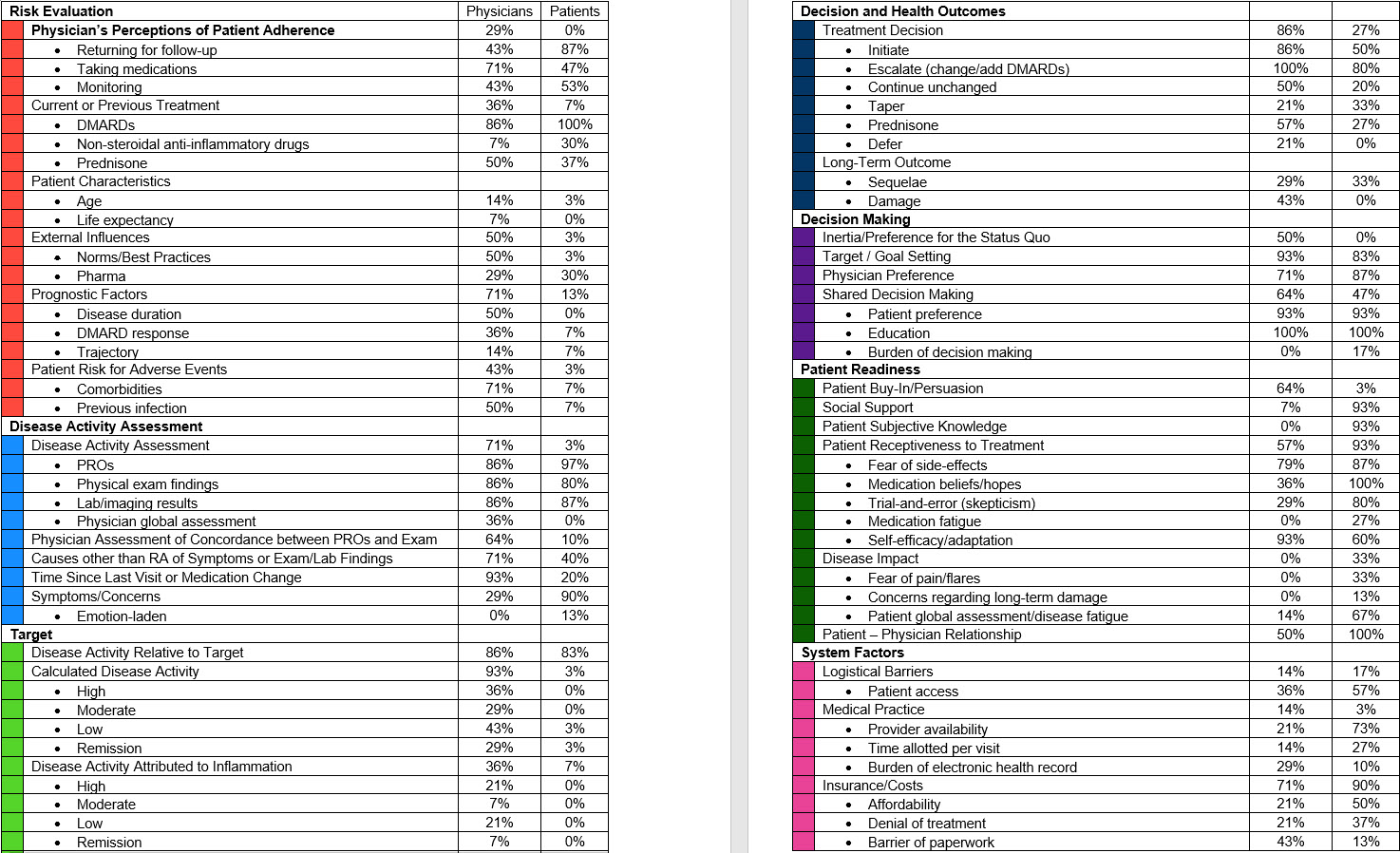
Methods: We conducted semi-structured interviews with 14 rheumatologists and 30 patients to elicit respondents’ views regarding treatment decisions in RA, with a focus on TTT. Interviews were transcribed and coded independently by two researchers. Final agreement between coders was high (kappa > 95%). We report the prevalence of each concept mentioned using the corresponding code. Because some ideas may not be expressed, these proportions represent a lower bound of their prevalence in people’s mental models.
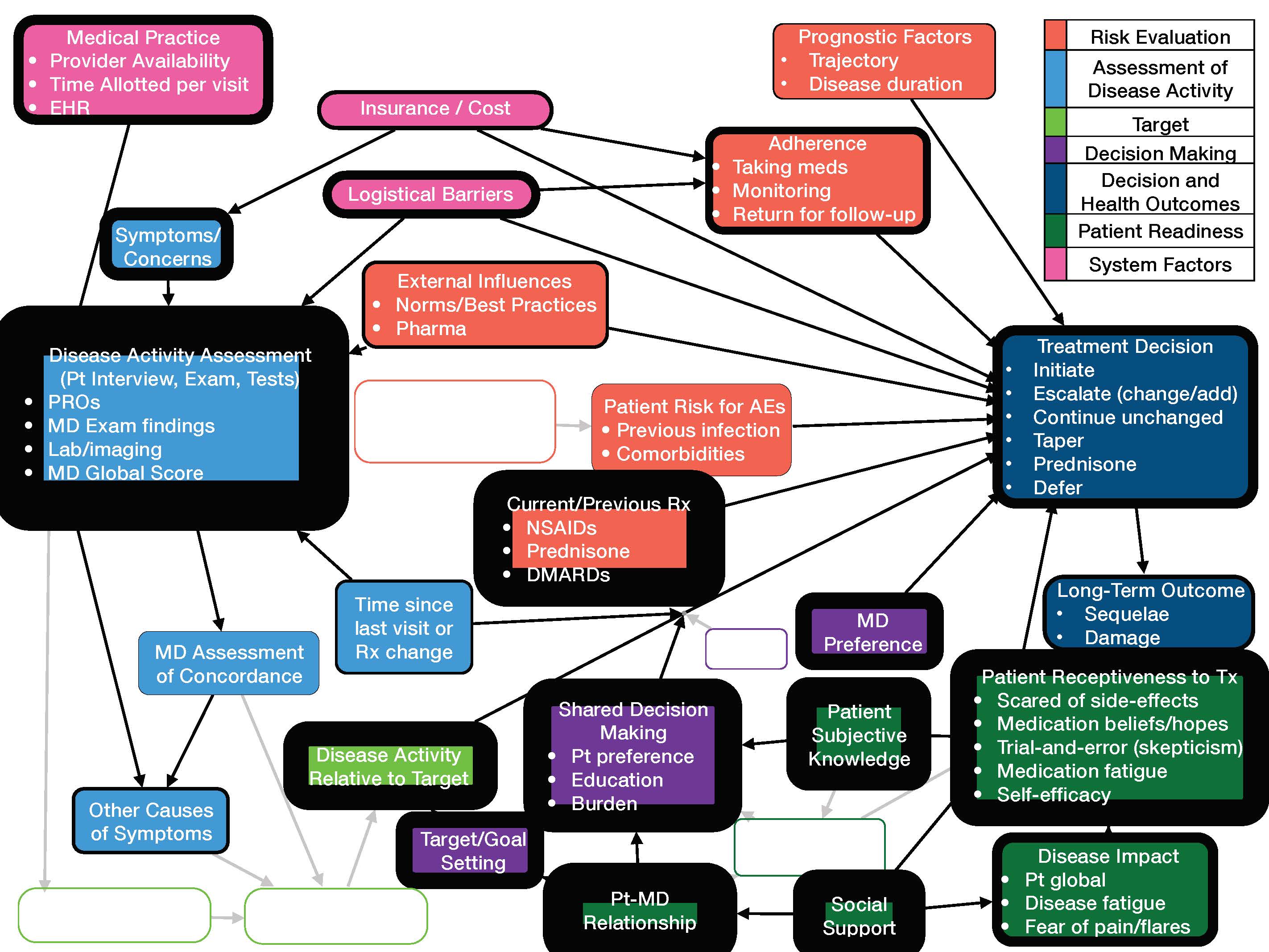
Results: Table 1 presents all factors raised in the interviews. Based on the codes assigned to each set of interviews, we created one model representing how rheumatologists conceptualize TTT (Figure 1) and another representing how patients conceptualize their treatment (Figure 2). Border thickness represent the frequency with which concepts were raised. Empty shapes highlight discrepancies between the rheumatologist and patient models. Several physicians stated that treatment decisions should be made based on overall trajectory of disease rather than at the point-of-care. They also described the importance of adherence and response to previous DMARDs on their decision making. Physicians recognized system barriers at the patient level (e.g., inadequate transportation), practice level, and insurance. Physicians also described how their own preferences and pharmaceutical company influences might affect their treatment decisions.
Notably absent from the patients’ mental model is the cornerstone of TTT, i.e., disease activity measurement using validated instruments. Patients’ anticipation of future experience on new medications. They described the necessity of feeling adequately informed, including from sources outside of their rheumatologist, in order to make treatment changes. Several discussed the burden of making treatment decisions. The uncertainty regarding whether one will benefit from a new DMARD and the risk of new side effects was frequently mentioned as an adverse aspect of changing medications. Concerns of the influence of pharmaceutical companies on rheumatologists’ recommendations were also raised.
Conclusion: The TTT model of care is specific and prescriptive: measure disease activity and adjust treatment to achieve or maintain a predefined target using shared decision making. However, rheumatologists’ and patients’ mental models of treatment decision making in RA are much more complex and explain the low rates of TTT implementation. We found several discrepancies primarily related to differences in how patients and physicians value trade-offs that can serve as specific targets to improve patient-physician communication and ultimately inform interventions to improve uptake of TTT.
To cite this abstract in AMA style:
Hsiao B, Downs J, Lanyon M, Nowell W, VENKATACHALAM S, Wiedmeyer C, Curtis J, Blalock S, Harrold L, Fraenkel L. Rheumatologists’ and Patients’ Mental Models for Treatment of RA Explain Low Rates of TTT [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/rheumatologists-and-patients-mental-models-for-treatment-of-ra-explain-low-rates-of-ttt/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rheumatologists-and-patients-mental-models-for-treatment-of-ra-explain-low-rates-of-ttt/