Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: African Americans and Hispanics with rheumatoid arthritis (RA) or systemic lupus erythematosus (SLE) continue to have worse disease-related health outcomes relative to Whites. This pilot study investigates the relationship between living in a disadvantaged neighborhood and the frequency of being prescribed a biologic agent or a conventional disease modifying rheumatic drug (DMARD). The objective of this study was to determine if a relationship exists between race/ethnicity, living in a disadvantaged neighborhood, and the frequency of being prescribed disease-specific treatment for RA or SLE.
Methods: Data from the electronic medical record (EMR) of a large urban hospital were analyzed for the period from January 1, 2020 through September 30, 2020. Independent variables included age, insurance information, address with zip code, race/ethnicity, and sex. The area deprivation index score was calculated using the neighborhood atlas website mapping tool. Rheumatologic medications were the dependent variables. Prescribed biologic agents or conventional DMARDs were compared between racial/ethnic groups. Prescriptions of steroids, non-steroidal medications, and opiates were also compared.
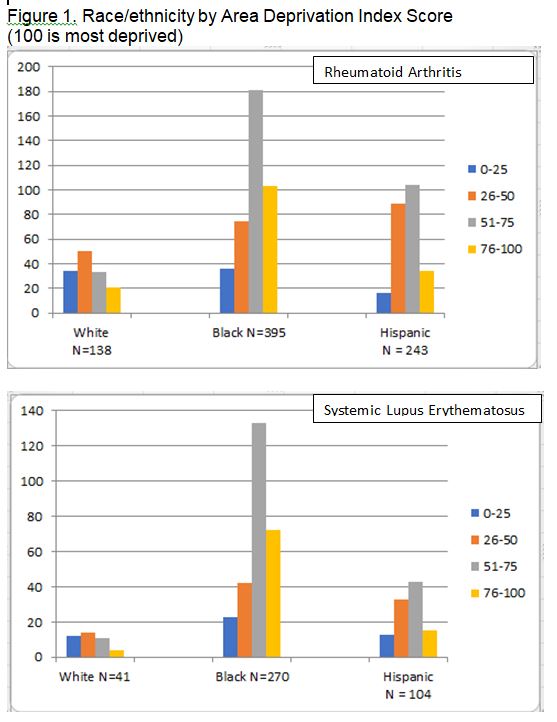
Results: Altogether there were 1326 unique patients with RA (n=859) or SLE (n=457). There were 181 non-Hispanic Whites, 671 non-Hispanic Blacks, and 347 Hispanic patients.
Area deprivation index scores were higher among Black and Hispanic patients compared to White patients for both RA and SLE patients (p < 0.00001 RA and SLE) . Minorities with RA were also more likely to have Medicaid health insurance than Whites (p < 0.00005 RA; p < 0.59 SLE ). Results showed that physician prescribing patterns did not vary with area deprivation index scores (p< 0.878 RA; p < 0.08 SLE).
Conclusion: Among patients with RA and SLE, Blacks and Hispanics are more likely to live in an area with a higher area deprivation index score. Black RA patients were more likely to have Medicaid as their insurance. Physician prescribing patterns did not vary with area deprivation scores. Future studies with larger sample sizes are needed to help quantify the relationships between area deprivation scores and insurance in order to better understand physician prescribing patterns in patients, particularly among minority groups living in these areas, and to understand how these factors may influence disease-related health outcomes in RA and SLE.
To cite this abstract in AMA style:
Berry J, Galanter W, Welsh A, Folarin S, Woods R, Chang H. Racial/Ethnic Disparities in Prescription Medications in a Large Urban Medical Center [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/racial-ethnic-disparities-in-prescription-medications-in-a-large-urban-medical-center/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-ethnic-disparities-in-prescription-medications-in-a-large-urban-medical-center/