Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Geographic disparities in the distribution and practice patterns of rheumatology providers may negatively impact patients with rheumatic diseases. The objective of this study was to describe the distribution of rheumatologists with respect to the area deprivation index (ADI) and to identify differences in practice patterns among Medicare Part D rheumatologist prescribers.
Methods: Prescriber data from the Medicare Part D Prescriber Public Use Files from 2013-2018 were downloaded. These data were joined to zip code level area deprivation index (ADI) data from the University of Wisconsin-Madison Neighborhood Atlas and presented as means and standard deviations (SDs). The ADI per zip code and number of rheumatologists per zip code were analyzed using Pearson’s correlation. The average number of rheumatologists and the average ADI values for each zip code were stratified by year and analyzed using one-way ANOVAs. Prescribing rates per 100 beneficiaries were calculated for corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs), gabapentinoids, opioids, conventional synthetic disease modifying anti-rheumatic drugs (csDMARDs), and targeted synthetic or biological (ts/bDMARDs) and analyzed using one-way ANOVAs.
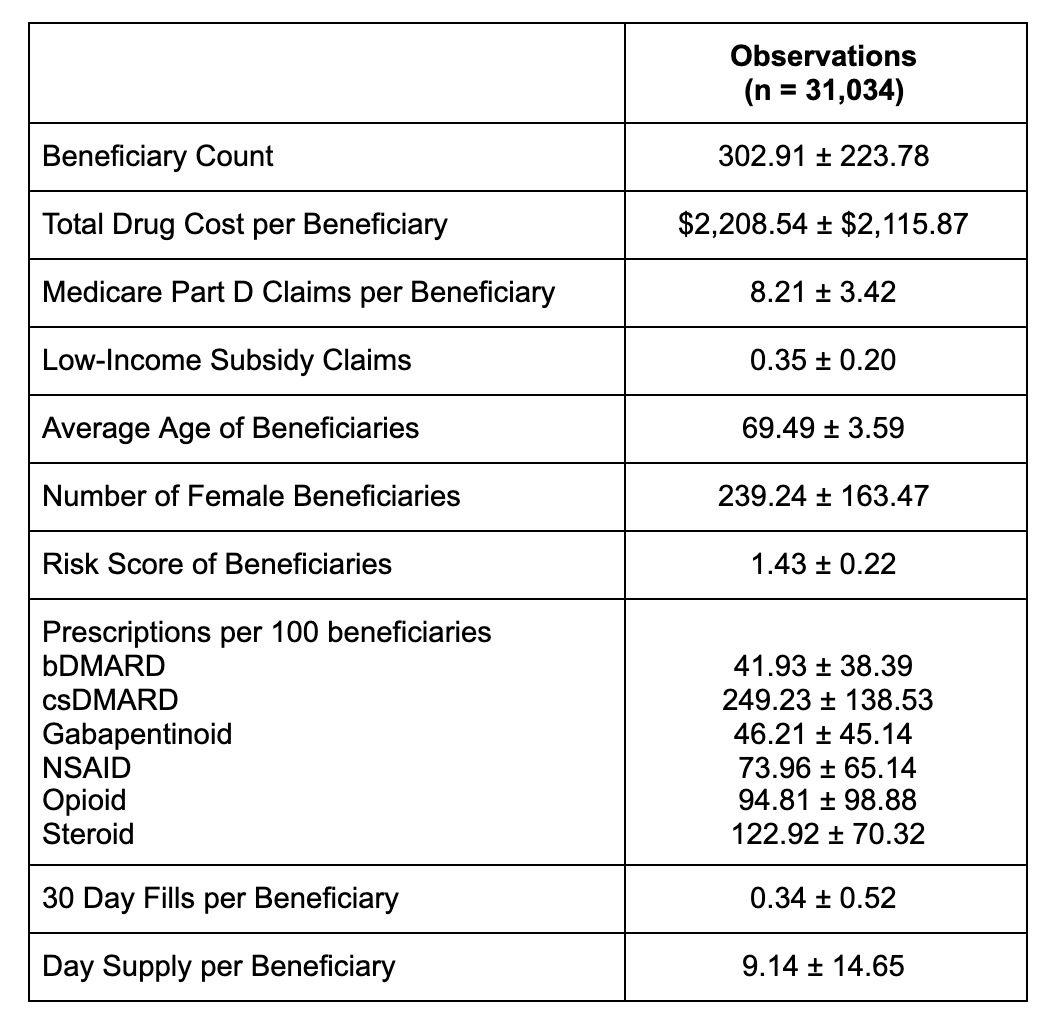
Results: This study identified 5,642 rheumatologists who participated in the Medicare Part D program from 2013 to 2018. These rheumatologists served an average of 302.9 +/- 223.8 beneficiaries with an average age of 69.5 +/- 3.6 years (Table 1). In an unadjusted linear model of the number of rheumatologists per zip code, there was no significant relationship with ADI (p = 0.159). In two one-way ANOVA models, there was no relationship between year and the average number of rheumatologists per zip code (p = 0.313) or the average ADI (p = 0.621) (Table 2). Per 100 beneficiaries, providers who practiced in a higher ADI quintiles cared for significantly more patients and prescribed more conventional synthetic disease modifying anti-rheumatic drugs, more gabapentinoids, and more opioids (p < 0.001 for all comparisons) (Table 3).
Conclusion: There was no significant association between the number of rheumatologists per zip code and the ADI per zip code. Rheumatologists who practice in zip codes with higher deprivation indexes saw more patients and prescribed more csDMARDS, more gabapentinoids, and more opioids. Prescribing rates for biologic and targeted synthetic DMARDs did not vary substantially, suggesting that access to health insurance may mitigate geographical disparities.
To cite this abstract in AMA style:
Tai S, Mbonu I, Putman M. Association of Area Deprivation Index and Practice Patterns of Medicare Part D Rheumatologists [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/association-of-area-deprivation-index-and-practice-patterns-of-medicare-part-d-rheumatologists/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-area-deprivation-index-and-practice-patterns-of-medicare-part-d-rheumatologists/