Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Health care disparities in hypertension and other chronic disease are well established. Ethnic minority residents of Washington DC, particularly Wards 7 and 8, have higher rates of chronic disease and shortened lifespans, but little is known about the impact on rheumatoid arthritis (RA) in these areas. The Ethnic Minority Rheumatoid Arthritis Consortium (Howard University Hospital –[HUH]) comprised of 9 sites nationwide, reported more severe RA disease, worse outcomes, and less use of biologic therapy. Further, socioeconomic factors were linked to delayed diagnosis, worse prognosticators/seropositivity and functional outcomes. Patient assessment of overall health and disease activity have been shown to correlate positively with RA outcomes, but may be influenced by non-RA factors such as comorbidities. HUH serves a primarily DC residential African American population. We evaluated the association of area of residence on perceptions of health and RA disease status.
Methods: EMRAC participants seen at HUH and with at least one follow-up visit were evaluated. The associations of sociodemographic factors and RA disease status with Wards/Area of residence, perception of health (poor, fair, good, excellent) and physical activity (seldom, monthly, weekly) were evaluated. Logistic regression models were used to estimate associations of patients’ perception of health and RA disease activity (RAPID3) within non-DC and DC regions, adjusting for gender, age, race, physical activity and comorbidities.
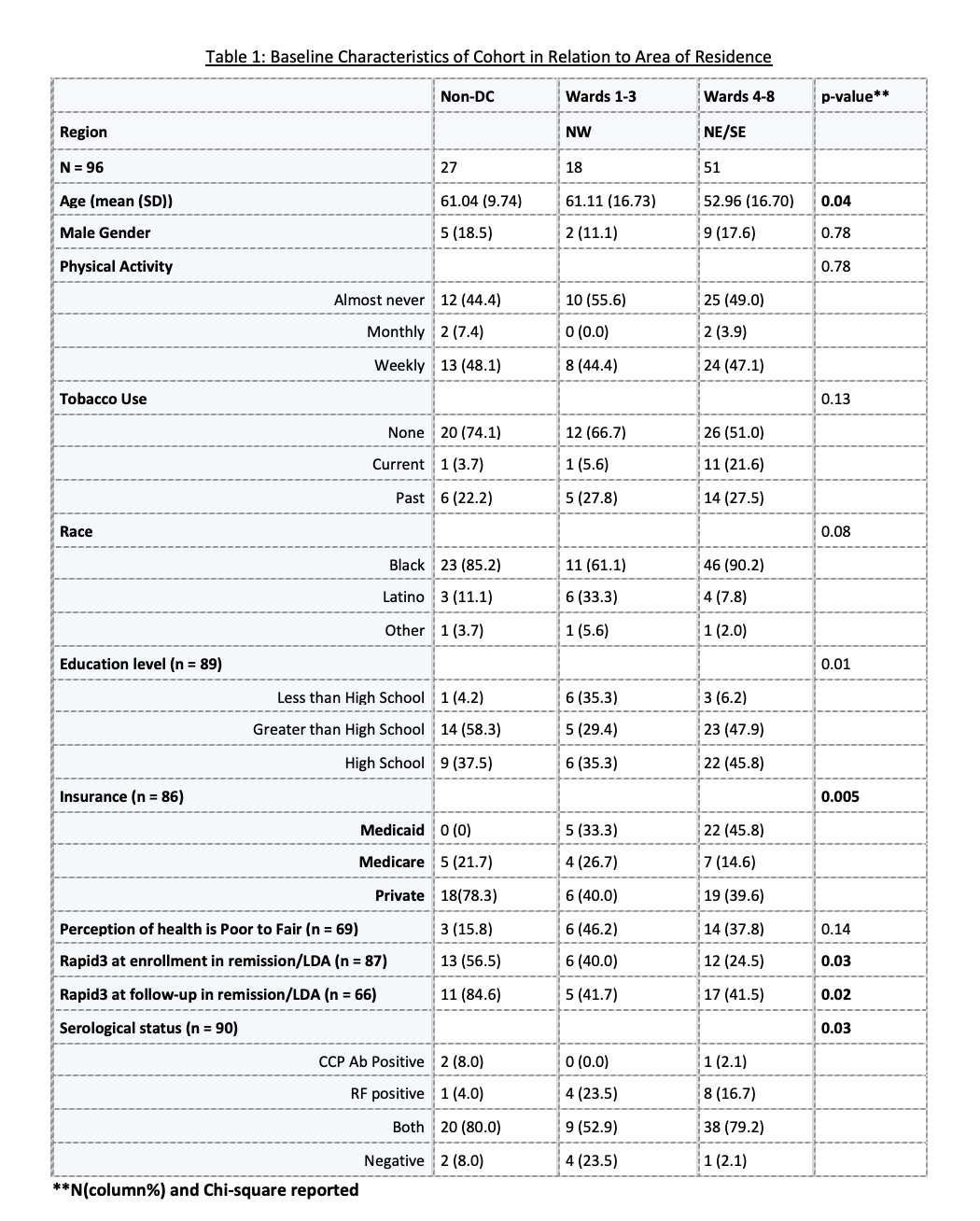
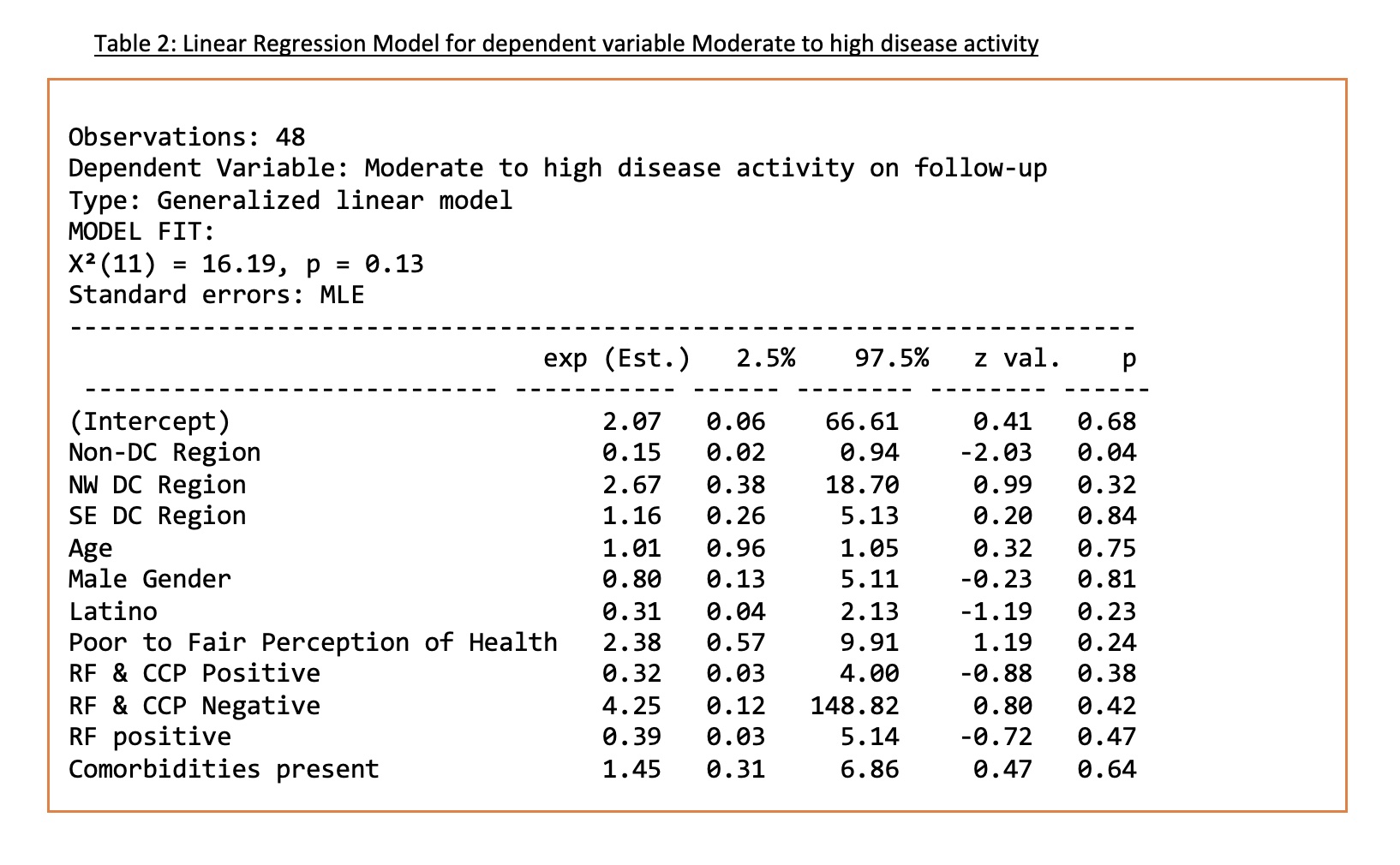
Results: An enrollment cohort of 96 EMRAC subjects (females 83%, mean age 55 years (SD 15.5) was available for analysis (Table 1.). Wards 4-8 corresponded to the NE, SE areas of DC and comprised of younger patients with more frequent seropositivity and higher disease activity compared to Wards 1-3 (NW, SW DC). Sixty-four percent (56/87) had moderate to high disease activity; of whom, 66% of whom were from Wards 4-8. More non-DC patients were in remission/low disease activity at baseline and at 18 months – 13/23 (56.5%) and 11/13 (84.6%) respectively. Of 69 DC residents, 46 patients reported good to excellent perception of health (7 NW, 13 NE, and 10 SE). Of the remaining 23 DC residents (who reported fair to poor health), 70% resided in NE, SE areas. Non-DC residents (84%) were more likely to have a good to excellent perception of health compared to DC residents. Insurance data were available for 86 patients, 5 (6%) had non-DC Medicare/Medicaid, 38 (44%) had DC Medicare/Medicaid, and 43 (50%) were privately insured. Weekly physical activity was positively associated with perception of good health, regardless of area of residence (p-value: 0.02). Logistic regression (Table 2), controlling for demographic factors, found low disease activity and a non-DC domicile was significant (p-value: 0.05).
Conclusion: RA patients in an urban region served by a single institution demonstrated differences in disease activity and perceptions of health based on area of residence. While physical activity may play a role in the perception of health it may not be solely explained by RA disease activity. Evaluation of the role of insurance coverage and physical activity in improving RA outcomes is a priority in this vulnerable population
To cite this abstract in AMA style:
Jalloh M, Dowell S, Ogunti R, Kerr G. Impact of Area of Residence on Perceptions of Health and Disease Activity in Ethnic Minorities with Rheumatoid Arthritis in an Urban Setting [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/impact-of-area-of-residence-on-perceptions-of-health-and-disease-activity-in-ethnic-minorities-with-rheumatoid-arthritis-in-an-urban-setting/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-area-of-residence-on-perceptions-of-health-and-disease-activity-in-ethnic-minorities-with-rheumatoid-arthritis-in-an-urban-setting/