Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: SLE is a chronic, multisystem autoimmune disease characterized by reoccurring flares and remissions. It is more common among Asian, Black, and Hispanic populations. Racial disparity in SLE disease burden, including socioeconomic status (SES), and quality of life (QOL), is not well described in SLE patients. Our study sought to characterize the prevalence of SLE, demographic characteristics, SES, QOL, and health care resource utilization between Black vs. White adults in the US.
Methods: We analyzed 2016 – 2018 Medical Expenditure Panel Surveys (MEPS). MEPS is an annual survey designed to represent the US civilian non-institutionalized population. MEPS oversamples specific racial minority groups to ensure adequate representation. Annual SLE respondents were identified using ICD-10 M32 and had to have either SLE-related medication or at least 1 rheumatologist visit during the calendar year to be included for analysis. Descriptive comparisons were pooled across all three years and stratified by Black, White or Other races, with results focusing on Black vs. White comparison.
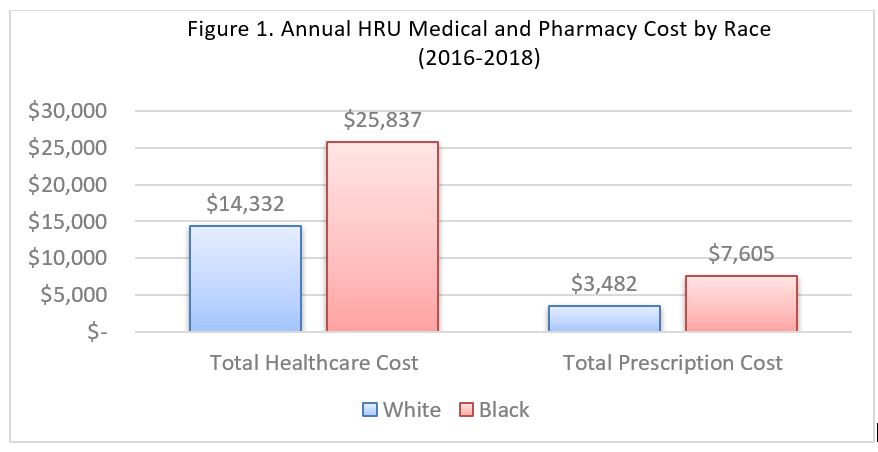
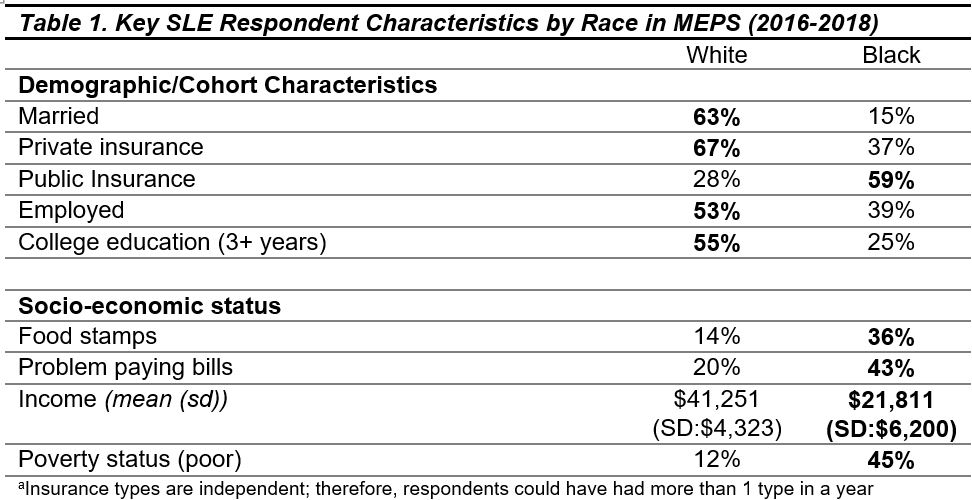
Results: The prevalence of SLE was higher in Black adults 287 (95% CI: 162, 412) per 100,000 compared to White adults 187 (95% CI: 133, 241) per 100,000. Black SLE respondents were younger (46.8 vs. 50.1 years old), less likely to be married (15% vs. 63%), less likely to have 3+ years of college education (24% vs. 55%), less likely to be employed (39% vs. 53%), and less likely be privately insured (37% vs. 67%) (Table 1). Black SLE respondents had a significantly higher prevalence of select comorbidities including arthritis (86% vs. 54%), diabetes (30% vs. 6%) , stroke (17% vs. 5%). MI (10% vs. 1%),and heart disease (27% vs. 19%). Black adults reported poorer overall health and health-limited activity, including the ability to work (Table 2). 52% Black adults (vs. 14% White) reported “completely unable to do activities.” White SLE respondents were 2–3 times less likely to report difficulty with physical limitations—including standing, walking, bending, and reaching. More Black respondents reported using antimalarial medication than White (80% vs. 57%), with no other differences in SLE-related medications. Overall, Black SLE respondents had higher annual healthcare expenses ($25,837 (95% CI 16,318 – $34,972) vs $14,332 (95% CI 9,551 – $19,112)) which were driven by higher costs within office visits and emergency room events. Prescription costs were also higher in Black compared to White respondents, although not statistically different.
Conclusion: In this survey population, when compared with White SLE adults, Black SLE adults were younger, presented with more comorbidities, reported more physical limitations, and higher expenses in emergency room visits and overall healthcare spending. These differences may adversely affect long-term outcomes, suggesting there is a continuing need to further assess racial disparities in SLE to improve outcomes for this population.
To cite this abstract in AMA style:
Grabich S, Seal C, Ortmann R, Sze-jung Wu S. Racial Disparities in US Adults with Systemic Lupus Erythematosus: Prevalence, Quality of Life, Comorbidities and Healthcare Costs [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/racial-disparities-in-us-adults-with-systemic-lupus-erythematosus-prevalence-quality-of-life-comorbidities-and-healthcare-costs/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-disparities-in-us-adults-with-systemic-lupus-erythematosus-prevalence-quality-of-life-comorbidities-and-healthcare-costs/