Session Information
Date: Sunday, November 7, 2021
Title: Systemic Sclerosis & Related Disorders – Basic Science Poster (0541–0559)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Pulmonary arterial hypertension (PAH) is a major clinical challenge in systemic sclerosis (SSc). It is associated with impaired quality of life and high mortality. In 2015, the treatment recommendations changed, recommending upfront combination therapy from the time of diagnosis. The objective of this study was to assess the impact of upfront dual combination therapy versus monotherapy on PAH progression and mortality.
Methods: We included all patients with SSc who had right heart catheterization (RHC) between 2005 and 2018 at Oslo University Hospital, and who were diagnosed with PAH, defined as a mean pulmonary arterial pressure (mPAP) ≥ 25 mmHg and a pulmonary artery wedge pressure ≤ 15mmHg in the absence of interstitial lung disease (ILD). Longitudinal clinical characteristics including treatment were assessed; vital status were available in all patients. To study treatment regimens over time, patients were categorized into three subgroups in regard to diagnostic periods. To secure that all patients had at least 3 years of follow up, group 1 consisted of patients diagnosed between 2005 and 2009, group 2 of patients diagnosed between 2010 and 2014, and group 3 of patients diagnosed between 2015 and 2018. Treatment was initiated as soon as PAH had been confirmed, and included (1) an endothelin-1 receptor antagonist (ERA) and/or (2) a phosphodiesterase-5 inhibitor (PDE5 inhibitor). To assess the impact of treatment regimens on mortality and PAH progression, two outcomes were assessed, including (1) death and (2) PAH-progression defined as a) intensified PAH treatment, b) increasing respiratory symptoms and/or c) hemodynamic progression defined as reduction in the cardiac index (CI) to less than 2.5 l/min/m2, or mixed venous oxygen saturation (SVO2) < 65%. We constructed Kaplan-Meier plots and performed time-to-event analyses.
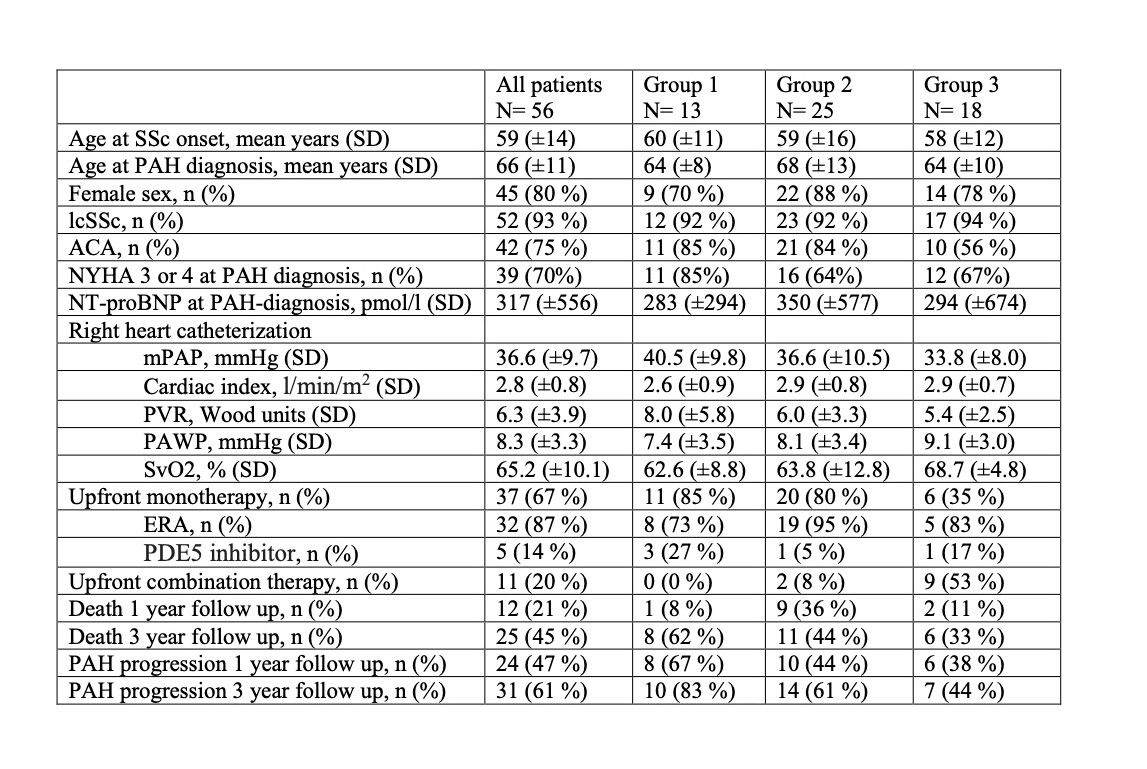
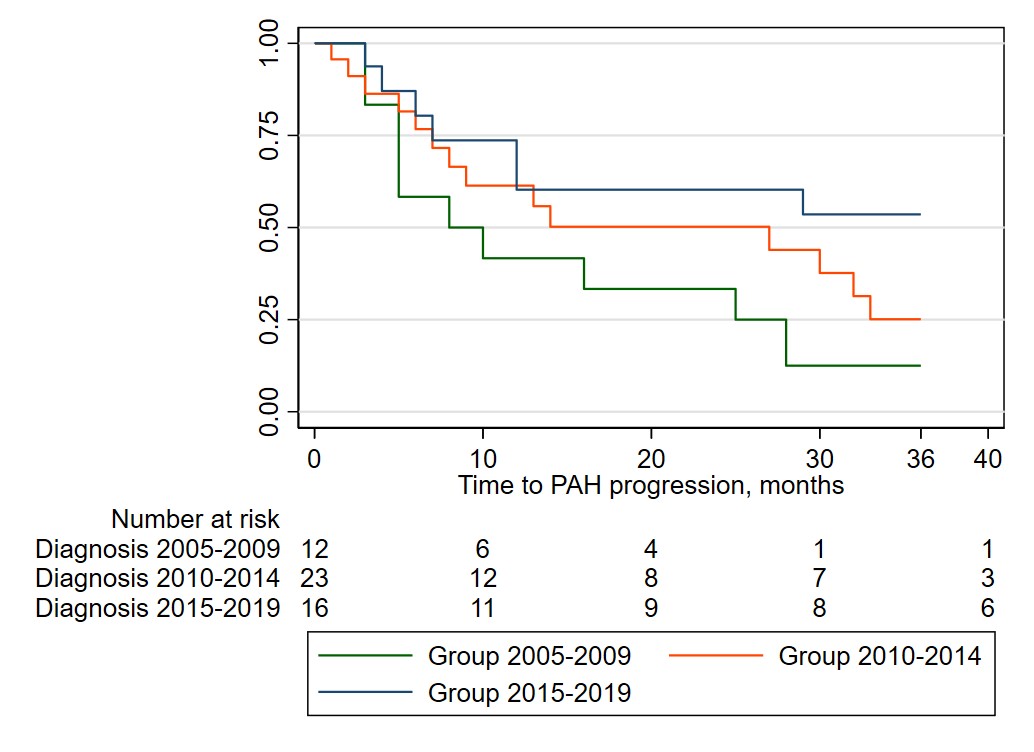
Results: In total, 191 patients had RHC in the study period, whereof 56 (29 %) SSc patients had a PAH diagnosis. Mean age at SSc-diagnosis was 59 years, mean age at PAH-diagnosis 66 years; 80 % were female and 93 % had limited cutaneous SSc (table 1). None of the patients in group 1 started upfront combination therapy compared to 53 % of patients in group 3. Event-free survival was better in group 3 compared to groups 1 and 2 as shown in the table and figure (p=0.05). 3-year survival increased numerically across groups 1 through 3, from 54% via 62% to 78% (p= 0.148).
Conclusion: We show that upfront dual combination therapy for SSc-PAH has been used more frequently after 2015 in Norway. This shift is associated with less progression of PAH and increased survival in patients with SSc-PAH. This may indicate that there is a benefit of upfront dual combination therapy in SSc-PAH patients in addition to higher awareness and better monitoring strategies.
To cite this abstract in AMA style:
Bjørkekjær H, Fretheim H, Inselseth H, Midtvedt , Barua I, Garen T, Bitter H, Andreassen A, Molberg , Broch K, Hoffmann-Vold A. Treatment Regimens and Outcomes in Systemic Sclerosis-associated Pulmonary Arterial Hypertension [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/treatment-regimens-and-outcomes-in-systemic-sclerosis-associated-pulmonary-arterial-hypertension/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/treatment-regimens-and-outcomes-in-systemic-sclerosis-associated-pulmonary-arterial-hypertension/