Session Information
Date: Saturday, November 6, 2021
Title: Abstracts: Healthcare Disparities in Rheumatology (0492–0495)
Session Type: Abstract Session
Session Time: 3:45PM-4:00PM
Background/Purpose: Longitudinal data are limited on SLE flare hospitalizations. This study aims to study longitudinal trends of SLE flare hospitalizations in the last 2 decades in the United States (U.S) using national population data.
Methods: Data were obtained from the National Inpatient Sample database (NIS), the largest hospitalization database in the U.S. We performed a 21-year longitudinal trend analysis of NIS 1998-2018. Every 5th year of the NIS during this study period was sampled. We obtained data from NIS 1998, 2003, 2008, 2013, and 2018 databases. We searched for hospitalizations for patients aged≥ 18 years with “principal” diagnosis of SLE using ICD 9 code “7100” or ICD 10 code “M32”. We defined an SLE flare hospitalization as one with a “principal” diagnosis of SLE. The “principal” diagnosis is the main reason for hospitalization. All hospitalizations for patients aged≥ 18 years were used as the control population. NIS underwent a redesign in 2012, hence revised trend weights were used to make estimates comparable across the years. Multivariable logistic and linear regression was used to calculate adjusted p-trend for categorical and continuous outcomes, respectively. We adjusted for changes in demographics and charlson comorbidity index (CCI) score over time. STATA version 16 was used for analysis.
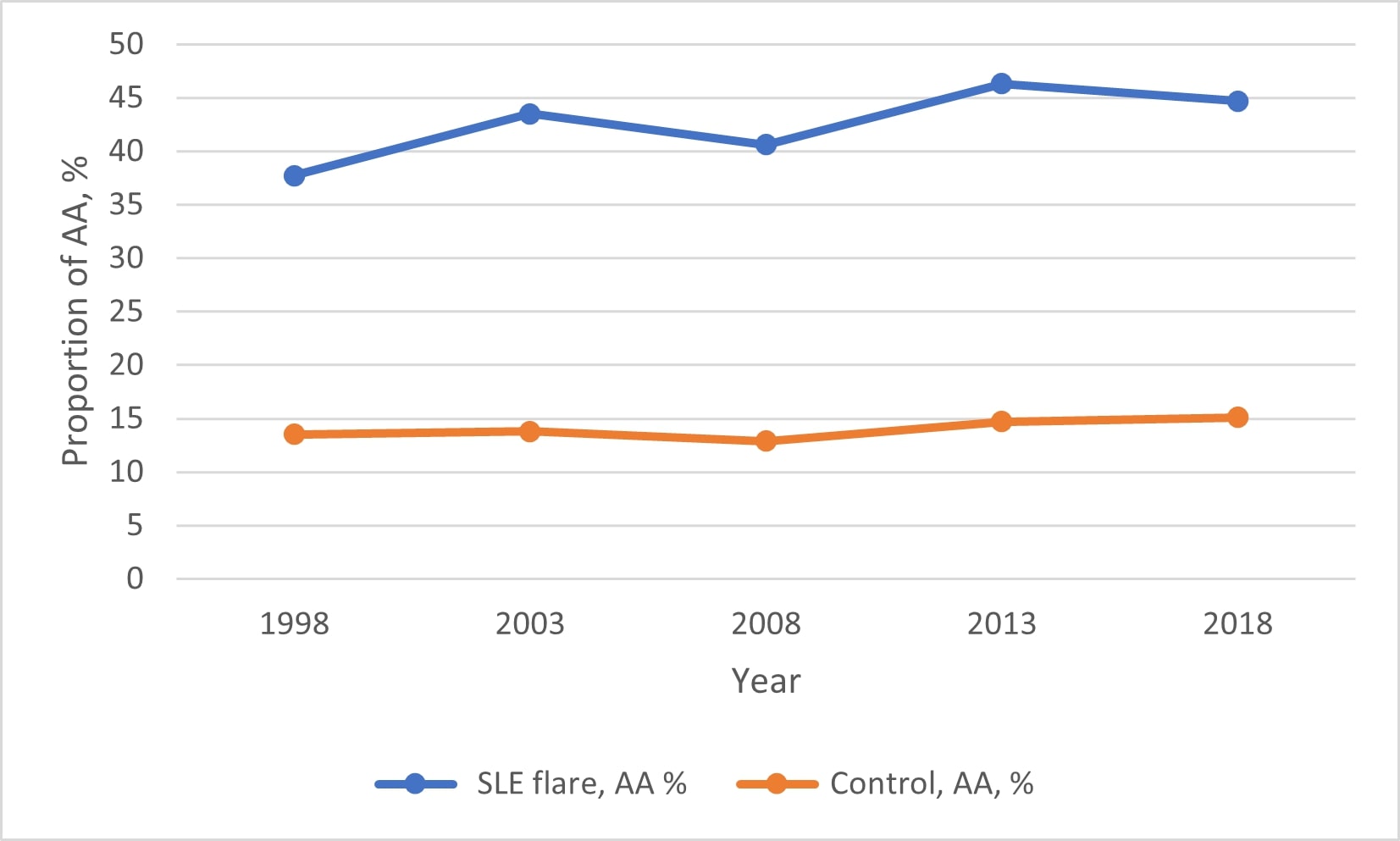
Results: Incidence of SLE flare hospitalization reduced from 4.1 per 100,000 in 1998 to 3.2 per 100,000 in 2018 (adjusted p-trend < 0.0001). See Figure 1. Proportion of hospitalized African American (AA) SLE flare hospitalizations increased from 37.7% in 1998 to 44.7% in 2018 (adjusted p-trend < 0.0001), while hospitalized AA in the control increased from 13.5% in 1998 to 15.1% in 2018 (adjusted p-trend=0.06). See Figure 2. Racial trends of other ethnic groups were similar between SLE flare and the control population. Hospital length of stay (LOS) reduced and total hospital charges and CCI score increased for both the SLE flare and control groups during our study period (Table 1).
Conclusion: The incidence of hospitalization for SLE flare has reduced in the last two decades in the U.S. This may reflect improving outpatient SLE flare recognition and management. Although AA makes up only 13-15% of the general adult hospitalized population, they constitute the majority of SLE flare hospitalizations (38-46%). The burden of SLE flare hospitalizations among AA has increased over the last 2 decades. This may reflect a lack of access to primary and specialist care among AA. More studies on racial disparities in SLE flare hospitalizations are needed.
Abbreviations: SLE, Systemic Lupus Erythematosus; USD, United States Dollars, I: Incidence per 100,000 persons, CCI, Charleston comorbidity index. p<0.005 was statistically significant.
* We included hospitalizations for patients aged ≥18 years with a principal diagnosis of SLE
* The incidence of SLE flare hospitalizations was calculated by dividing the number of SLE hospitalizations in the NIS by the population estimate of the U.S on July 1 of the corresponding year. The population estimates were obtained from the U.S Census Bureau Website
*** All hospital charges were adjusted for inflation by using the medical expenditure panel survey-based factor for hospital care and were presented in 2018 United States dollars (USD).
All adult hospitalizations aged ≥ 18 years was used as the control population
To cite this abstract in AMA style:
Edigin E, Eseaton P, Osuorji C, Chukwu N, Amoda O, Olabode K, Manadan A. Hospitalization for SLE Flare Has Reduced over Two Decades in the United States: A Longitudinal Population-based Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/hospitalization-for-sle-flare-has-reduced-over-two-decades-in-the-united-states-a-longitudinal-population-based-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hospitalization-for-sle-flare-has-reduced-over-two-decades-in-the-united-states-a-longitudinal-population-based-study/