Session Information
Date: Saturday, November 6, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Diagnosis (0323–0356)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Classification criteria for systemic lupus erythematosus (SLE) were recently published by the European League Against Rheumatism (EULAR) and American College of Rheumatology (ACR) to reflect current diagnostic approaches and improve statistical performance with addition of entry criterion and item weighting. The validation cohort included a small proportion of African American patients, a population disproportionately affected by early and severe SLE. We evaluated the performance of the EULAR/ACR 2019 criteria within a predominantly African American well-characterized cohort of patients with SLE.
Methods: Patients enrolled in a single center longitudinal prospective study of SLE were included, excluding patients without a confirmed expert clinical rheumatologist diagnosis of SLE. Demographic, clinical, and immunologic features were compared between the EULAR/ACR Classification Criteria for SLE and the 1997 ACR criteria. Chart review was completed for missing values. Fulfilling criteria for SLE was defined as the presence ≥4 ACR criteria or ≥10 points for the EULAR/ACR criteria. ”Any damage” on the Systemic Lupus International Collaborating Clinics (SLICC) Damage Index is a score ≥1 and “high damage” is a score ≥2.
Results: A total of 682 patients with SLE were included. Of the 682 patients, 524 identified as black (76.3%), 20 as non-black Hispanic (2.9%), and 90.6% female. Patients with childhood onset SLE (diagnosed at ≤ 18 years) comprised 18.3% of the cohort. A proportion of the SLE patients have an additional overlapping autoimmune disease (n=166, 30.7%) most commonly Sjogren’s, RA, or autoimmune thyroid disease. SLICC damage was present in 63.6% of patients (n=434), with 42.5% (n=290) having high damage. The mean 1997 ACR criteria score was 5.6 (median 5) out of 11 possible. The mean EULAR/ACR criteria score was 20.6 (median 20) out of 51 possible.
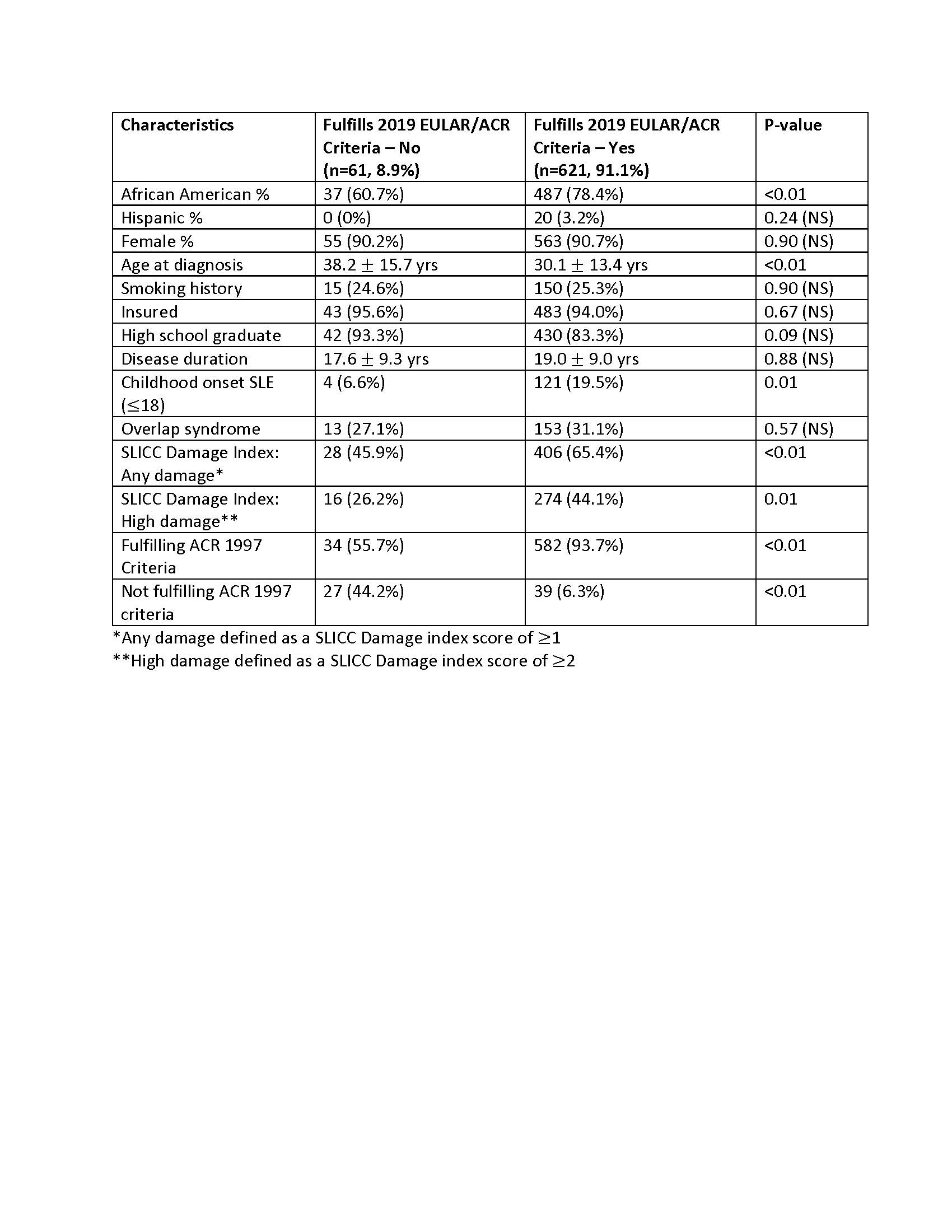
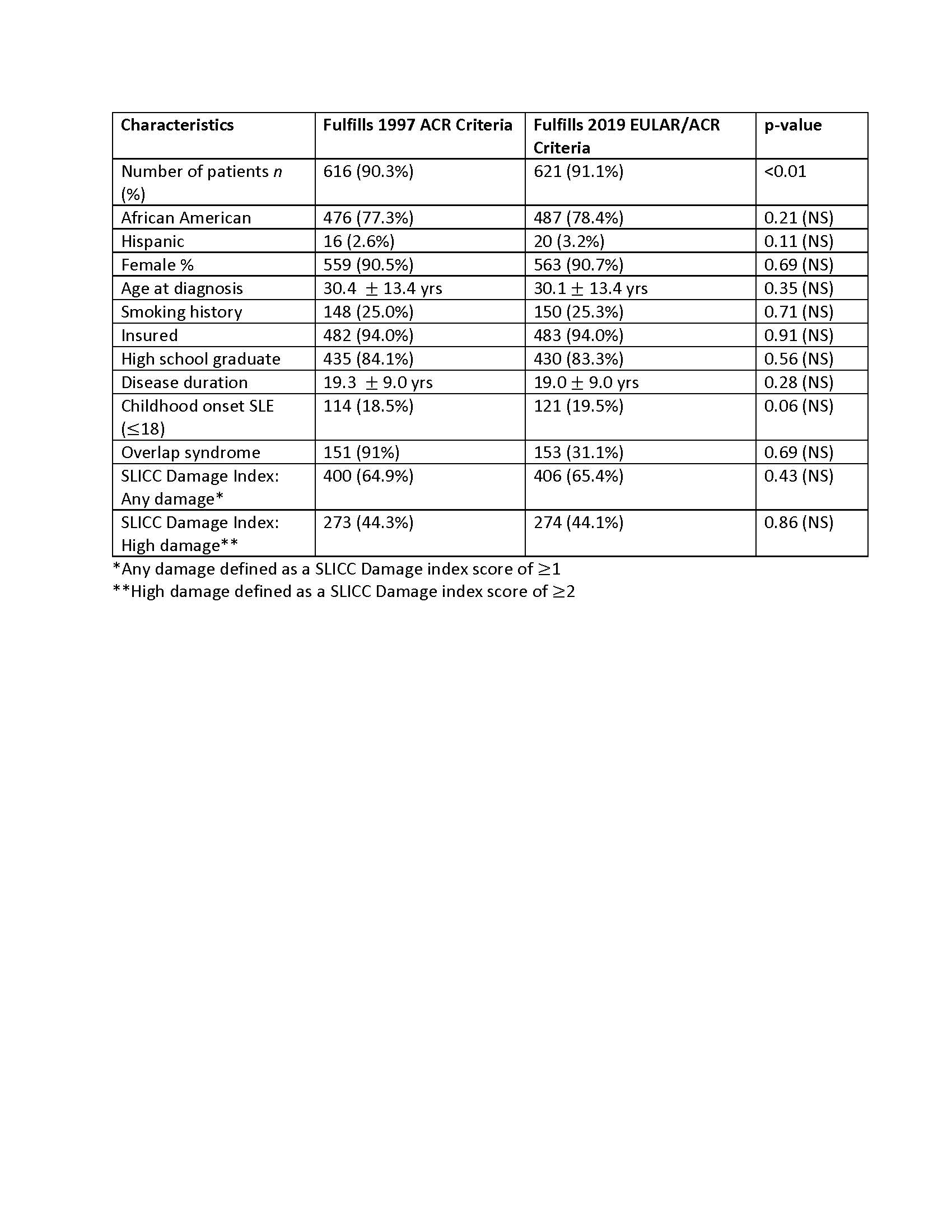
Table 1 compares patients fulfilling EULAR/ACR criteria to the 8.9% who did not. Table 2 compares patients fulfilling ACR criteria to those fulfilling EULAR/ACR criteria. Of patients who meet ACR criteria, blacks were more likely to meet EULAR/ACR criteria compared to whites (96.4% vs 87.9%, respectively, p< 0.01). EULAR/ACR criteria had a sensitivity of 91.1% overall (92.9% among black patients, p< 0.01) and the ACR criteria had sensitivity of 90.3% overall (90.8% among black patients, p< 0.01). Contributing to this gap were differences in ANA positivity (99.0% of blacks compared to 96.2% of non-blacks, p=0.01) and lupus nephritis, especially Class III and IV by biopsy (59.5 % of blacks compared to 33.5% of non-blacks, p< 0.01).
Conclusion: In this cohort of predominately African American patients with SLE, the sensitivities of the ACR 1997 criteria and EULAR/ACR 2019 criteria differed significantly by race. ANA positivity as an entry criterion, in addition to higher weighting for renal disease, accounts for some of the higher sensitivity of the EULAR/ACR criteria among African Americans. The importance of knowing the performance characteristics of these criteria, particularly for African American patients, cannot be understated, as the need for identifying patients for early intervention is critical.
To cite this abstract in AMA style:
English J, Wilson D, Gilkeson G, Oates J, Kamen D. Performance of the 2019 EULAR/ACR Classification Criteria for Systemic Lupus Erythematosus in a Predominantly African American Cohort [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/performance-of-the-2019-eular-acr-classification-criteria-for-systemic-lupus-erythematosus-in-a-predominantly-african-american-cohort/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/performance-of-the-2019-eular-acr-classification-criteria-for-systemic-lupus-erythematosus-in-a-predominantly-african-american-cohort/