Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: The relationship between serum lipoproteins and cardiovascular (CV) disease risk in rheumatoid arthritis (RA) is complex. Their levels and function may vary based on disease activity and medication use. Treatment benefits on high-density lipoprotein (HDL) levels, structure and behavior, in response to treatment have been described. Yet, the impact of HDL-C levels over time on coronary atherosclerosis progression in RA is unknown. We here evaluated the influence of HDL-C levels over time on long-term coronary plaque formation and progression in RA.
Methods: One hundred one patients without CV disease who underwent computed tomography angiography study of coronary atherosclerosis had repeat assessments after 6.9±0.3 years to evaluate plaque progression. Clinical, laboratory and medication data were captured at baseline and throughout follow-up. Robust logistic regression assessed associations between time-averaged HDL-C and likelihood of new plaque formation in segments without plaque at baseline, and transition of partially calcified to fully calcified plaque. Robust multinomial logistic regression evaluated effects of time-averaged HDL-C on likelihood of new noncalcified, partially or fully calcified plaque in segments without plaque (compared to remaining without plaque), and noncalcified plaque regression or transition to partially or fully calcified plaque (compared to remaining noncalcified). Models accounted for clustering of segments within patients and adjusted for Framingham CV risk score, segment location, time-averaged CRP, prednisone dose, bDMARD and statin duration, obesity, and time-averaged triglycerides.
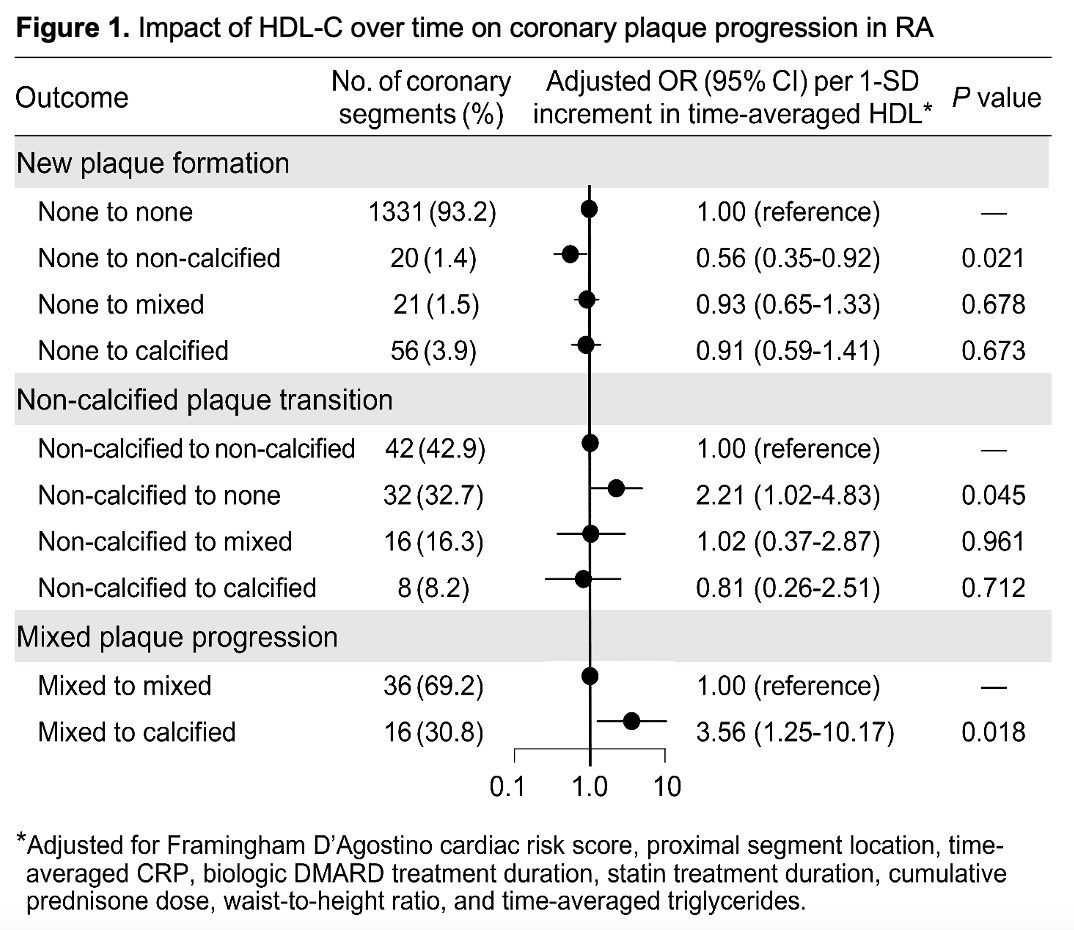
Results: Participants were mostly female (n=87, 86.1%), 51.5±10.3 years old and time-averaged HDL-C was 51.7±13.9. Ninety-seven new plaques formed in segments without baseline plaque; 20 were noncalcified, 21 partially, and 56 were fully calcified. Time-averaged HDL-C had no effect on new total plaque formation (adjusted OR 0.88 [95% CI 0.64-1.21]). However, each SD increase in time-averaged HDL-C associated with a 44% lower chance of new noncalcified plaque (adjusted OR 0.56 [95% CI 0.35-0.92], Figure 1); no effect on incident partially or fully calcified plaque was observed. Of 98 noncalcified plaques at baseline, 42 remained unchanged, 32 regressed, 16 transitioned to partially and 8 to fully calcified plaques. Each SD increase in time-averaged HDL-C yielded a 2.2-fold greater chance of noncalcified plaque regression (adjusted OR 2.21 [95% CI 1.02-4.83]). Sixteen of 52 partially calcified plaques transitioned to fully calcified lesions; each SD increment in time-averaged HDL-C) predicted 3.5-fold greater odds of transition of partially to fully calcified plaque (adjusted OR 3.56 [95% CI 1.25-10.17]).
Conclusion: Higher HDL-C over time predicted regression of existing and decreased formation of new higher-risk noncalcified plaque. It also associated with transition of partially calcified to more stable fully calcified plaque. All effects were independent of RA treatment duration, prednisone dose and statin exposure.
To cite this abstract in AMA style:
Karpouzas G, ormseth s, Hernandez E, Budoff M. Greater High-density Lipoprotein Levels over Time Are Linked to Lower Coronary Plaque Formation, Regression and Stabilization of High-risk Lesions in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/greater-high-density-lipoprotein-levels-over-time-are-linked-to-lower-coronary-plaque-formation-regression-and-stabilization-of-high-risk-lesions-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/greater-high-density-lipoprotein-levels-over-time-are-linked-to-lower-coronary-plaque-formation-regression-and-stabilization-of-high-risk-lesions-in-rheumatoid-arthritis/