Session Information
Date: Saturday, November 6, 2021
Title: Health Services Research Poster I: Lupus, Inflammatory Arthritis, & More (0128–0148)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: The clinical presentation of systemic lupus erythematosus (SLE) is complicated, as patients cycle through periods of active disease (flares) and remission. To establish the burden of SLE, the heterogenous nature of the population must also be taken into consideration, particularly as it relates to the frequency and nature of flare treatment. The purpose of this study was to assess and characterize the annual rate of SLE flares by the site of care where treated (inpatient hospital [IP], emergency room [ER], and outpatient [OP]), and to observe the progression of specific flare rates and types in a subsequent year.
Methods: SLE patients were selected from IBM MarketScan commercial claims and encounters databases between 1/1/2013–3/31/2019. Inclusion criteria: 1) ≥1 inpatient claim with a diagnosis for SLE, or ≥2 non-diagnostic SLE outpatient claims with at least one rheumatologist or nephrologist specialty designation (index date set to a random SLE service date with ≥12 months of SLE disease history preceding it to create a prevalence cohort), 2) continuous enrollment with medical and pharmacy benefits for 12 months pre- and post-index, and 3) valid steroid Rx claims. SLE flares were defined using a published claims-based algorithm based on presence of SLE-related treatment and diagnosis1; results were presented during the 12-month period preceding (year 1) and following index (year 2). Flare progression from year 1 to year 2 were observed among four mutually exclusive cohorts of patients who had >1 flare treated in IP, >1 flare in ER but no IP, >1 flare in OP but no IP/ER, and no flares in year 1.
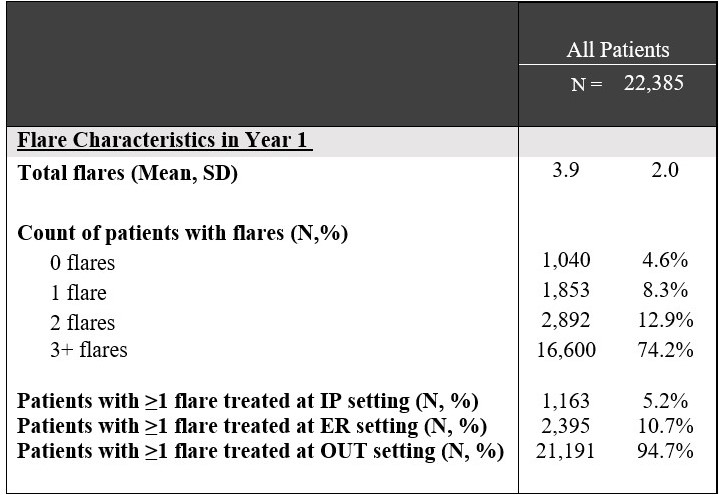
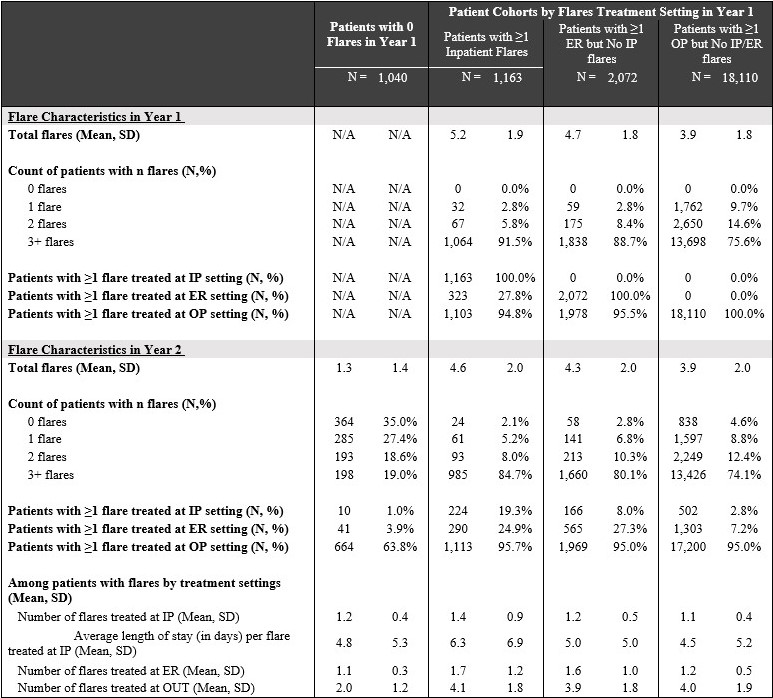
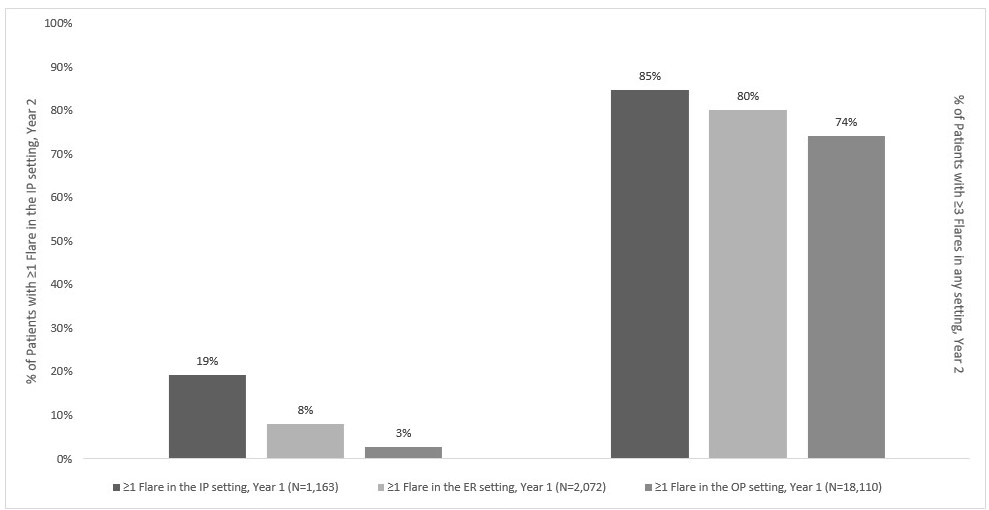
Results: 22,385 SLE patients qualified for the study; 95.4% (N=21,345) presented >1 flare in year 1; 5.4% (n=1,163) were treated in the IP, 9.7% (n=2,072) in the ER, and 84.8% (n=18,110) in an OP setting. Nearly 2/3 of patients without a flare in year 1 presented a flare in year 2, with 19.0% presenting >3 flares (Table 1). Among patients with a flare in year 1, 75.3% presented >3 flares in year 2. Compared to patients without a year 1 flare, those with a prior-year flare were more likely to present year 2 flares in the IP (4.2% vs. 1.0%), ER (10.1% vs. 3.9%), and OP (71.2% vs. 34.6%). Analyses segmented by baseline flare site of care revealed that, among patients with a flare treated in the IP setting, 19.3% presented an IP flare in year 2, and 24.9% presented an ER flare, substantially higher than patients without prior-year flares treated in the IP (Table 2). Compared to patients with baseline flares in the ER or OP settings, those with baseline flares in the IP setting were more likely to present >3 flares in that same year (84.7% vs. 80.1% and 74.1%; Figure 1).
Conclusion: Rates of SLE flares vary by patient subgroups over time and by flare history. SLE patients with more resource-intensive flares may be more likely to experience additional flares of similar or worse intensity in the future. An accurate assessment of disease flares is critical to quantifying the burden of SLE, and can inform the development of treatment options to control disease and minimize healthcare burden at the population level. Results highlight a potential unmet need in the current treatment landscape.
1. Garris C, et al. J Med Econ. 2013;16(5):667-677.
To cite this abstract in AMA style:
Sze-jung Wu S, Perry A, Varker H, Bizier R, Tkacz J, Ortmann R. Real-World Flare Rates and Progression by Treatment Settings Among the Commercially-Insured Systemic Lupus Erythematosus Population in the U.S [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/real-world-flare-rates-and-progression-by-treatment-settings-among-the-commercially-insured-systemic-lupus-erythematosus-population-in-the-u-s/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/real-world-flare-rates-and-progression-by-treatment-settings-among-the-commercially-insured-systemic-lupus-erythematosus-population-in-the-u-s/