Session Information
Session Type: Abstract Session
Session Time: 10:00AM-10:50AM
Background/Purpose: To assess whether comorbid diseases frequently associated with primary hospitalizations for non-vasculitis causes in people with vasculitis are changing over time in people with vasculitis in the U.S.
Methods: We identified people with vasculitis hospitalized with a non-primary/secondary diagnosis of vasculitis in the 1998-2014 U.S. National Inpatient Sample (NIS). We compared the rank (and percent) of top 25 Clinical Classification Software (CCS) categories (a standardized system for clustering diagnoses and procedures) associated with hospitalizations and in-hospital mortality in people with vasculitis, between 1998-99 versus 2013-14.
Results: In 1998-99, there were 69,170 non-primary vasculitis hospitalizations compared to 86,720 in 2013-14. The top 5 CCS categories associated with non-primary vasculitis hospitalizations in people with vasculitis in 1998-99 were circulatory system disease, heart disease, digestive system disease, respiratory disease, and musculoskeletal disease (Ranks 1-5 in order, respectively; Figure 1). In 2013-2014, the top 5 CCS (and change in rank from 1998-1999) categories were circulatory system disease (rank #1 to #1), infections/parasitic diseases (rank #10 to #2), bacterial infection (rank #11 to #3), septicemia (rank #12 to #4), and unspecified septicemia (rank #18 to #5; Figure 1). Compared to 27.7% non-primary vasculitis hospitalizations associated with circulatory system disease in 1998-99, 21.3% were associated in 2013-14.
In 1998-99, there were 817 deaths during non-primary vasculitis hospitalizations in people with vasculitis compared to 766 in 2013-14. The top 5 CCS categories associated with in-hospital death for non-primary vasculitis hospitalizations in 1998-99 were respiratory disease, circulatory system disease, heart disease, respiratory infection and pneumonia (Ranks 1-5 in order, respectively; Figure 2). In 2013-2014, these were infections/parasitic diseases (rank #6 to #1), bacterial infection (rank #7 to #2), septicemia (rank #9 to #3), unspecified septicemia (rank #22 to #4), and circulatory system disease (rank #1 to #5; Figure 2). In 1998-99, the top 3 CCS categories were all cardio-pulmonary diseases; in 2013-14, the top three CCS categories were all infections (Figure 2). Compared to 26.4% non-primary vasculitis hospitalization deaths associated with circulatory system disease in 1998-99, 20.5% were associated in 2013-14.
Conclusion: Infectious causes replaced cardio-pulmonary disease over time as the top causes of non-primary vasculitis hospitalizations and associated in-hospital mortality in people with vasculitis. Future studies should examine the modifiable factors associated with infection in vasculitis and design interventions to reduce this burden.
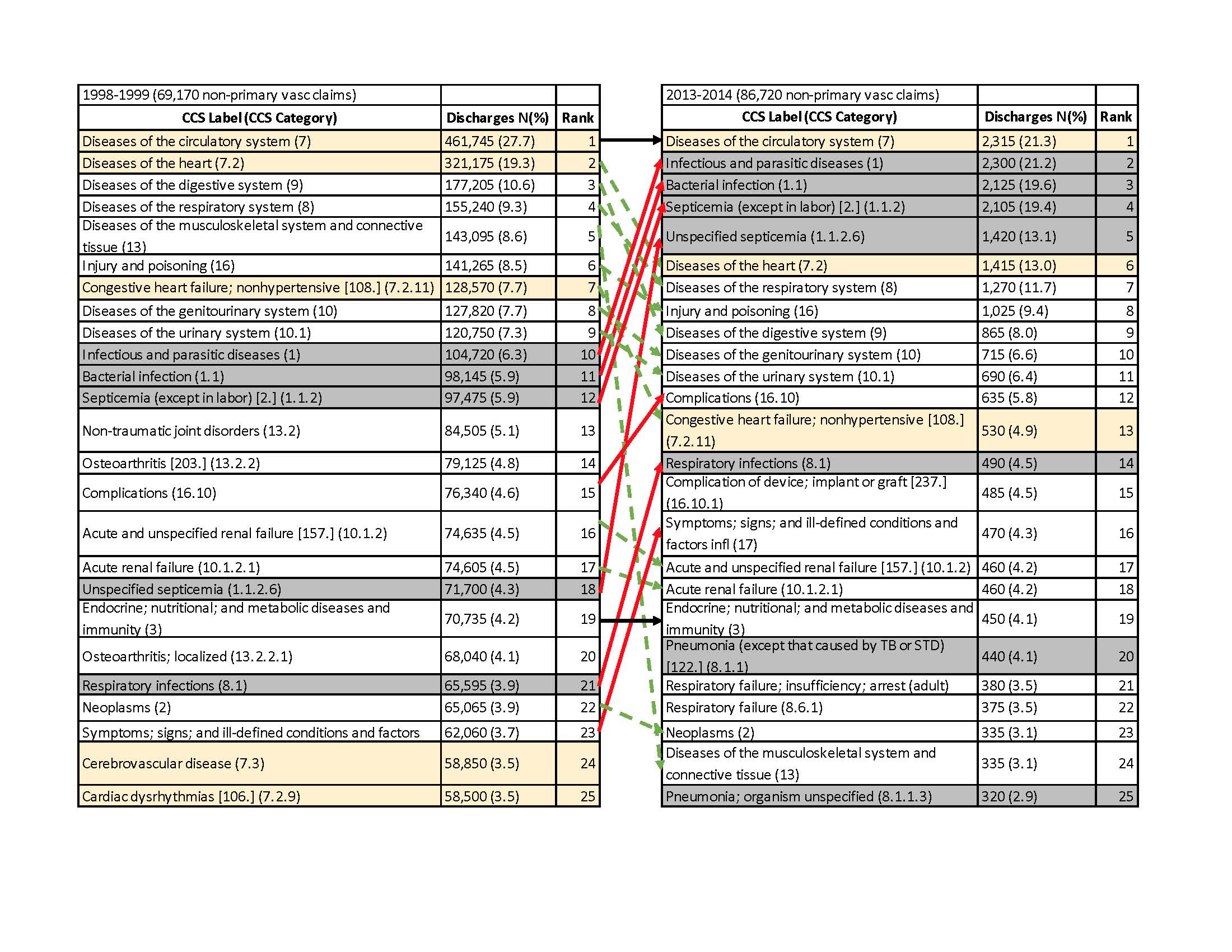 Figure 1. Top 25 healthcare cost and utilization project (HCUP) Clinical Classifications Software (CCS) categories for hospitalizations in people with vasculitis, comparing 1998-1999 to 2013-2014, with respective ranks Figure 1 legend The figure shows the top 25 CCS categories for hospitalization for the first period, 1998-1999 (left) and the last study period, 2013-2014 (right). Each CCS category label and category are shown in the first column, followed by the number and percent of discharges of all hospitalizations in the next column, followed by the relative rank from 1-25. Square brackets show the single-level CCS categories and regular brackets show multi-level CCS categories. Red arrows indicate any category that went to a higher rank in 2013-2014 and green indicates those any category that descended to a lower rank in 2013-2014. Solid black arrows show the categories whose rank remained the same. Number of discharges (percent) for each CCS category and rank is shown next to each CCS category. CCS categories included diagnoses in primary or non-primary position with vasculitis in non-primary position for hospitalizations in people with vasculitis. CCS consists of two related classification systems, single-level and multi-level. Single-level CCS system classifies all diagnoses and procedures. The single-level diagnosis CCS aggregates illnesses and conditions into 285 mutually exclusive categories. Most of these categories are homogeneous; for example, CCS category #100 is “Acute myocardial infarction and #101 is “Coronary atherosclerosis and other heart disease”. Some CCS categories combine several less common, individual conditions, such as CCS category #3, which is “Other Bacterial Infections. Similarly, the single-level procedure CCS aggregates procedures into 231 mutually exclusive categories, most representing single types of procedures. For example, #43 is “Heart valve procedures”, #44 is “Coronary artery bypass graft (CABG)” and #45 is “Percutaneous transluminal coronary angioplasty (PTCA)”. The multi-level CCS expands the single-level CCS into a hierarchical system. The multi-level CCS groups single-level CCS categories into broader body systems or condition categories. It also splits single-level CCS categories to provide more detail. The multi-level system has four levels for diagnoses and three levels for procedures, which provide the opportunity to examine general groupings or to assess very specific conditions and procedures.
Figure 1. Top 25 healthcare cost and utilization project (HCUP) Clinical Classifications Software (CCS) categories for hospitalizations in people with vasculitis, comparing 1998-1999 to 2013-2014, with respective ranks Figure 1 legend The figure shows the top 25 CCS categories for hospitalization for the first period, 1998-1999 (left) and the last study period, 2013-2014 (right). Each CCS category label and category are shown in the first column, followed by the number and percent of discharges of all hospitalizations in the next column, followed by the relative rank from 1-25. Square brackets show the single-level CCS categories and regular brackets show multi-level CCS categories. Red arrows indicate any category that went to a higher rank in 2013-2014 and green indicates those any category that descended to a lower rank in 2013-2014. Solid black arrows show the categories whose rank remained the same. Number of discharges (percent) for each CCS category and rank is shown next to each CCS category. CCS categories included diagnoses in primary or non-primary position with vasculitis in non-primary position for hospitalizations in people with vasculitis. CCS consists of two related classification systems, single-level and multi-level. Single-level CCS system classifies all diagnoses and procedures. The single-level diagnosis CCS aggregates illnesses and conditions into 285 mutually exclusive categories. Most of these categories are homogeneous; for example, CCS category #100 is “Acute myocardial infarction and #101 is “Coronary atherosclerosis and other heart disease”. Some CCS categories combine several less common, individual conditions, such as CCS category #3, which is “Other Bacterial Infections. Similarly, the single-level procedure CCS aggregates procedures into 231 mutually exclusive categories, most representing single types of procedures. For example, #43 is “Heart valve procedures”, #44 is “Coronary artery bypass graft (CABG)” and #45 is “Percutaneous transluminal coronary angioplasty (PTCA)”. The multi-level CCS expands the single-level CCS into a hierarchical system. The multi-level CCS groups single-level CCS categories into broader body systems or condition categories. It also splits single-level CCS categories to provide more detail. The multi-level system has four levels for diagnoses and three levels for procedures, which provide the opportunity to examine general groupings or to assess very specific conditions and procedures.
 Figure 2. Top 25 healthcare cost and utilization project (HCUP) Clinical Classifications Software (CCS) categories for In-hospital death for hospitalizations in people with vasculitis, comparing 1998-1999 to 2013-2014 Figure 2 legend The figure shows the top 25 CCS categories for In-hospital death for hospitalizations for the first period, 1998-1999 (left) and the last study period, 2013-2014 (right). Each CCS category label and category are shown in the first column, followed by the number and percent of discharges of all hospitalizations in the next column, followed by the relative rank from 1-25. Square brackets show the single-level CCS categories and regular brackets show multi-level CCS categories. Red arrows indicate any category that went to a higher rank in 2013-2014 and green indicates those any category that descended to a lower rank in 2013-2014. Solid black arrows show the categories whose rank remained the same. Number of discharges (percent) for each CCS category and rank is shown next to each CCS category.
Figure 2. Top 25 healthcare cost and utilization project (HCUP) Clinical Classifications Software (CCS) categories for In-hospital death for hospitalizations in people with vasculitis, comparing 1998-1999 to 2013-2014 Figure 2 legend The figure shows the top 25 CCS categories for In-hospital death for hospitalizations for the first period, 1998-1999 (left) and the last study period, 2013-2014 (right). Each CCS category label and category are shown in the first column, followed by the number and percent of discharges of all hospitalizations in the next column, followed by the relative rank from 1-25. Square brackets show the single-level CCS categories and regular brackets show multi-level CCS categories. Red arrows indicate any category that went to a higher rank in 2013-2014 and green indicates those any category that descended to a lower rank in 2013-2014. Solid black arrows show the categories whose rank remained the same. Number of discharges (percent) for each CCS category and rank is shown next to each CCS category.
To cite this abstract in AMA style:
Singh J, Cleveland J. Epidemiology of Hospitalizations and Associated Mortality in Vasculitis: A National Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/epidemiology-of-hospitalizations-and-associated-mortality-in-vasculitis-a-national-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/epidemiology-of-hospitalizations-and-associated-mortality-in-vasculitis-a-national-study/
