Session Information
Date: Monday, November 9, 2020
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Diagnosis of axial spondyloarthritis (axSpA) is challenging because of absent physical findings in early disease and the limited diagnostic performance of laboratory markers. Considerable reliance is placed on imaging of the sacroiliac joints (SIJ). We aimed to identify what might be the primary unmet educational needs of rheumatologists completing fellowship training within the past 6 years (post-F) by using clinical and imaging data from an inception cohort of consecutive patients presenting with undiagnosed back pain. We hypothesized that concordance between post-F rheumatologists and axSpA experts would increase after imaging data is reviewed following the clinical data.
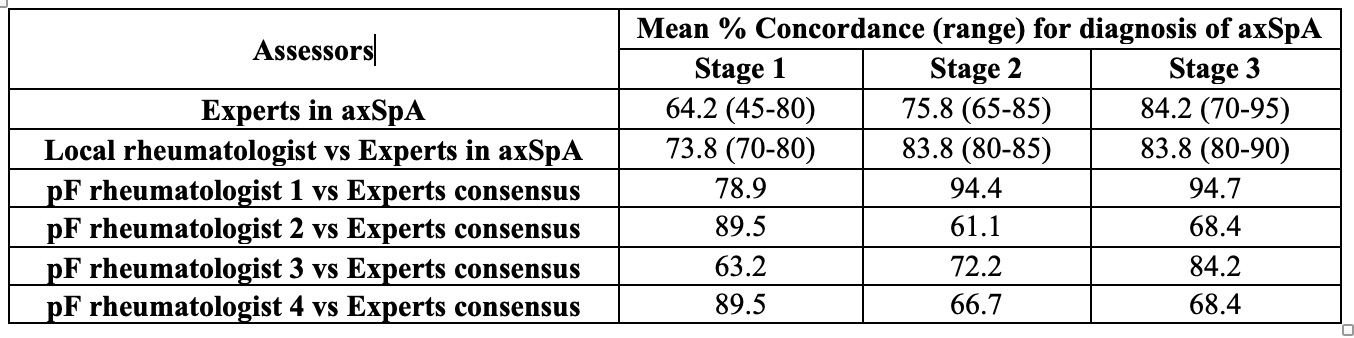
Methods: The diagnosis of axSpA was compared between local site rheumatologists recruiting patients for the cohort, axSpA experts who reviewed the diagnostic ascertainments, and post-F rheumatologists who assessed clinical and imaging data from the multicenter Screening for Axial Spondyloarthritis in Psoriasis, Iritis, and Colitis (SASPIC) Study. In this inception cohort, consecutive patients ≤45 years of age with ≥3 months undiagnosed back pain undergo routine diagnostic evaluation by a local SASPIC rheumatologist, including imaging of the SIJ, who then records a global evaluation of presence/absence of axial SpA. This is done at 3 consecutive stages: 1.After the clinical evaluation. 2.After the results of labs (HLA B27, CRP) and radiography. 3.After review of the local MRI report. In this exercise, 20 cases were selected from the SASPIC cohort with an equal distribution of axSpA and non-axSpA cases. Four experts in axSpA reviewed the clinical and imaging data in each eCRF in a sequential manner and provided their global diagnostic evaluations blinded to the assessments of local site rheumatologists for stages 1, 2, and 3 of these 20 cases. Subsequently, 4 post-F rheumatologists conducted the same exercise blinded to the assessments of the local site rheumatologist and experts in axSpA. Concordance (% agreement) between the assessors was analyzed.
Results: Diagnosis of axSpA by the local SASPIC rheumatologist was made in 90%, 65%, and 75% of cases after stages 1, 2, and 3, respectively. Majority diagnosis of axSpA by experts was made in 84.2% (16/19), 57.9% (11/19), and 63.2% (12/19), after stages 1,2, and 3, respectively. Majority diagnosis of axSpA by post-F rheumatologists was made in 94.4% (17/18), 100% (16/16), and 93.8% (15/16). Concordance among experts and between experts and local SASPIC rheumatologists increased after review of imaging data. For post-F rheumatologists concordance with experts increased after review of imaging for 2 assessors and decreased for the other 2 assessors. For the latter, the primary reason for decrease in concordance with experts was false positive diagnosis of axSpA in 35% and 30% of the cases after review of the imaging.
Conclusion: A structured case-based and sequential evaluation of clinical and imaging data suggests a gap in the training of recently graduated rheumatologists, with over-interpretation of imaging leading to false positive diagnosis of axSpA.
To cite this abstract in AMA style:
Maksymowych W, Caplan L, Deodhar A, Dolatabadi S, Hwang M, Carlson A, Steed K, Carapellucci A, Paschke J, Gensler L. Diagnosis of Axial Spondyloarthritis: A Primary Unmet Educational Need for Rheumatologists Is Interpretation of MRI [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/diagnosis-of-axial-spondyloarthritis-a-primary-unmet-educational-need-for-rheumatologists-is-interpretation-of-mri/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/diagnosis-of-axial-spondyloarthritis-a-primary-unmet-educational-need-for-rheumatologists-is-interpretation-of-mri/