Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Prior studies suggest women with SLE and RA may have higher age-adjusted risk of adverse pregnancy outcomes. We evaluated maternal and fetal complications and racial/ethnic disparities among pregnant women with SLE and RA using a national sample of hospital admissions.
Methods: We used the National Inpatient Sample (NIS), which after weighting provides annual estimates for more than 35 million community hospitalizations in the US. Analysis was limited to pregnant women without missing relevant variables hospitalized in 2016 and 2017. Admissions with SLE and RA were captured in ICD-10-CM codes (M32.1x, M32.8, M32.9 and M05, M06.0, M06.2, M06.8, M06.9, M08.0 respectively). We compared the proportion of discharge outcomes with maternal death, intrauterine fetal demise (IUFD), preeclampsia/eclampsia, premature rupture of membranes (PROM), and placental complications (placental disorders, placenta previa, or abruptio placentae) among patients with SLE, RA, and neither condition using chi-squared tests. We used Poisson regression to model outcomes as a function of disease, including age, race/ethnicity, insurance, and income level in the ZIP Code of residence as covariates. To evaluate racial/ethnic disparities across disease groups, we included an interaction term for race/ethnicity and disease (SLE, RA, neither) if the interaction was significant in the model. Weighted population estimates are presented, except if otherwise specified. All analyses accounted for the complex sampling design of the NIS.
Results: An estimated 11,100 (0.15%) community hospital admissions for pregnant women with SLE, 10,065 (0.13%) with RA, and 7,612,897 for women with neither condition occurred in the U.S. in 2016 and 2017. Maternal death was a rare event, accounting for less than 10 observations for admissions with either SLE or RA, and approximately 0.01% of general pregnancy related admissions. Admissions with a diagnosis of IUFD, preeclampsia/eclampsia, and placental complications were more likely among patients with SLE than the general pregnant population (p< 0.05) (Table 1). Similarly, admissions for patients with RA were more likely to have a diagnosis of preeclampsia/eclampsia, PROM, and placental complications compared to the general pregnant population (p< 0.05). The risk of IUFD and preeclampsia/eclampsia was higher among Blacks compared to whites (p< 0.05) both among the general pregnant population and those with SLE, but not among those with RA (Table 2).
Conclusion: Pregnant patients with SLE and RA have worse maternal and fetal outcomes including increased risk of intrauterine fetal demise, preeclampsia/eclampsia, PROM, or placental complications compared to other hospitalized pregnant women. Admitted pregnant Black patients with SLE, like those in the general population, continue to be at higher risk of poor maternal and fetal outcomes compared to whites. In contrast, there was no significant difference in the risk of analyzed maternal and fetal complications for Black compared to white RA patients. Women with SLE and RA continue to be at increased risk of pregnancy complications suggesting that additional obstetric research and interventions are indicated to improve outcomes in these patients.
 IUFD = intrauterine fetal demise; PROM = premature rupture of membranes; placental complications include ICD-10-CM codes for placental disorders, placenta previa, or abruptio placentae. Percent of discharges based on marginal predictions from adjusted Poisson model. RR= adjusted relative risk obtained from Poisson model including age, race, income quartile in ZIP Code of residence, insurance as covariates. Models for IUFD and preeclampsia/eclampsia also include an interaction term for race/ethnicity and disease. Ref = reference group. *Signifies statistical significance, p < 0.05. n weighted based on NIS guidelines to generate national estimates.
IUFD = intrauterine fetal demise; PROM = premature rupture of membranes; placental complications include ICD-10-CM codes for placental disorders, placenta previa, or abruptio placentae. Percent of discharges based on marginal predictions from adjusted Poisson model. RR= adjusted relative risk obtained from Poisson model including age, race, income quartile in ZIP Code of residence, insurance as covariates. Models for IUFD and preeclampsia/eclampsia also include an interaction term for race/ethnicity and disease. Ref = reference group. *Signifies statistical significance, p < 0.05. n weighted based on NIS guidelines to generate national estimates.
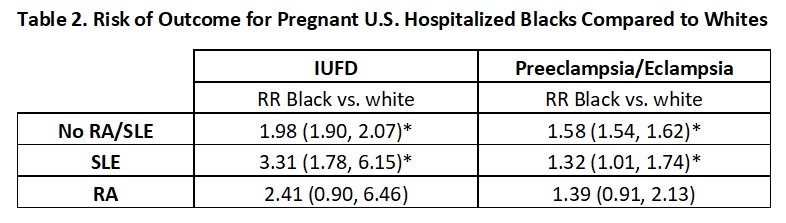 IUFD = intrauterine fetal demise; PROM = premature rupture of membranes; placental complications include ICD-10-CM codes for placental disorders, placenta previa, or abruptio placentae. RR= adjusted relative risk obtained from Poisson model including age, race, income quartile in ZIP Code of residence, insurance as covariates, and an interaction term for race/ethnicity and disease. *Signifies statistical significance, p < 0.05.
IUFD = intrauterine fetal demise; PROM = premature rupture of membranes; placental complications include ICD-10-CM codes for placental disorders, placenta previa, or abruptio placentae. RR= adjusted relative risk obtained from Poisson model including age, race, income quartile in ZIP Code of residence, insurance as covariates, and an interaction term for race/ethnicity and disease. *Signifies statistical significance, p < 0.05.
To cite this abstract in AMA style:
Anastasiou C, Trupin L, Katz P, Izadi Z, Gianfrancesco M, Schmajuk G, Yazdany J. Worse Maternal and Fetal Outcomes Among Hospitalized U.S. Pregnant Women with Systemic Lupus Erythematosus (SLE) and Rheumatoid Arthritis (RA) [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/worse-maternal-and-fetal-outcomes-among-hospitalized-u-s-pregnant-women-with-systemic-lupus-erythematosus-sle-and-rheumatoid-arthritis-ra/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/worse-maternal-and-fetal-outcomes-among-hospitalized-u-s-pregnant-women-with-systemic-lupus-erythematosus-sle-and-rheumatoid-arthritis-ra/
