Session Information
Date: Monday, November 9, 2020
Title: Pediatric Rheumatology – Clinical Poster III: SLE, Vasculitis, & JDM
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: The presence of antiphospholipid antibodies, including lupus anticoagulant (LA), is a risk factor for development of venous thromboembolism (VTE) in children. The impact of transient LA positivity on clinical outcomes of VTE are unknown. We investigated (1) the association of clinical outcomes with LA positivity at VTE diagnosis in the acute and chronic VTE phases and (2) the impact of LA at VTE diagnosis with fibrinolysis in the acute and chronic VTE phases.
Methods: We utilized a nested case-control study design to identify pediatric cases (VTE patients with positive LA at VTE diagnosis) and controls (VTE patients without LA at VTE diagnosis) nested within an ongoing prospective cohort study. Patients without a known lupus anticoagulant status within 4 weeks of VTE were excluded. We assessed participants for a composite clinical outcome of persistent veno-occlusion, recurrent VTE, or post-thrombotic syndrome (PTS) at 12 months post-diagnosis and a translational outcome of fibrinolysis capacity using a modified thromboelastography at 3- and 12-months post-diagnosis. We examined demographic and clinical characteristics between the cases and controls by univariate analysis and constructed a multivariable logistic regression model to identify predictors of our outcomes in LA positive patients.
Results: We identified 50 controls and 28 cases in our cohort. Baseline characteristics between both groups were similar with the exception of a higher BMI in the LA positive group (Table 1). Children with LA positivity at VTE diagnosis were more likely to present with thrombosis at multiple sites (46% vs. 18%, p=0.0074) and more likely to develop the composite clinical outcome (46% vs. 22% p=0.025) despite LA resolution at follow-up (Figure 1). In children with transient LA positivity, complete veno-occlusion and multi-site involvement at VTE diagnosis predicted the composite clinical outcomes at 12 months post-diagnosis. (Figure 2). No difference in fibrinolysis was observed at 3 months, but LA positive children were hypofibrinolytic at 12 months; this was not associated with BMI.
Conclusion: We present the first evidence that hypercoagulability induced by transient LA is prognostic in pediatric VTE. Children with LA positivity, even if transient, represent a unique subset of patients with adverse VTE outcomes in the acute and chronic VTE phases independent of inherited thrombophilia, inflammatory and infectious states. Larger studies are needed to validate our findings and to investigate if LA positive children require higher intensity of anticoagulation or upfront thrombolysis in the acute VTE phase to prevent adverse outcomes in the chronic phase.
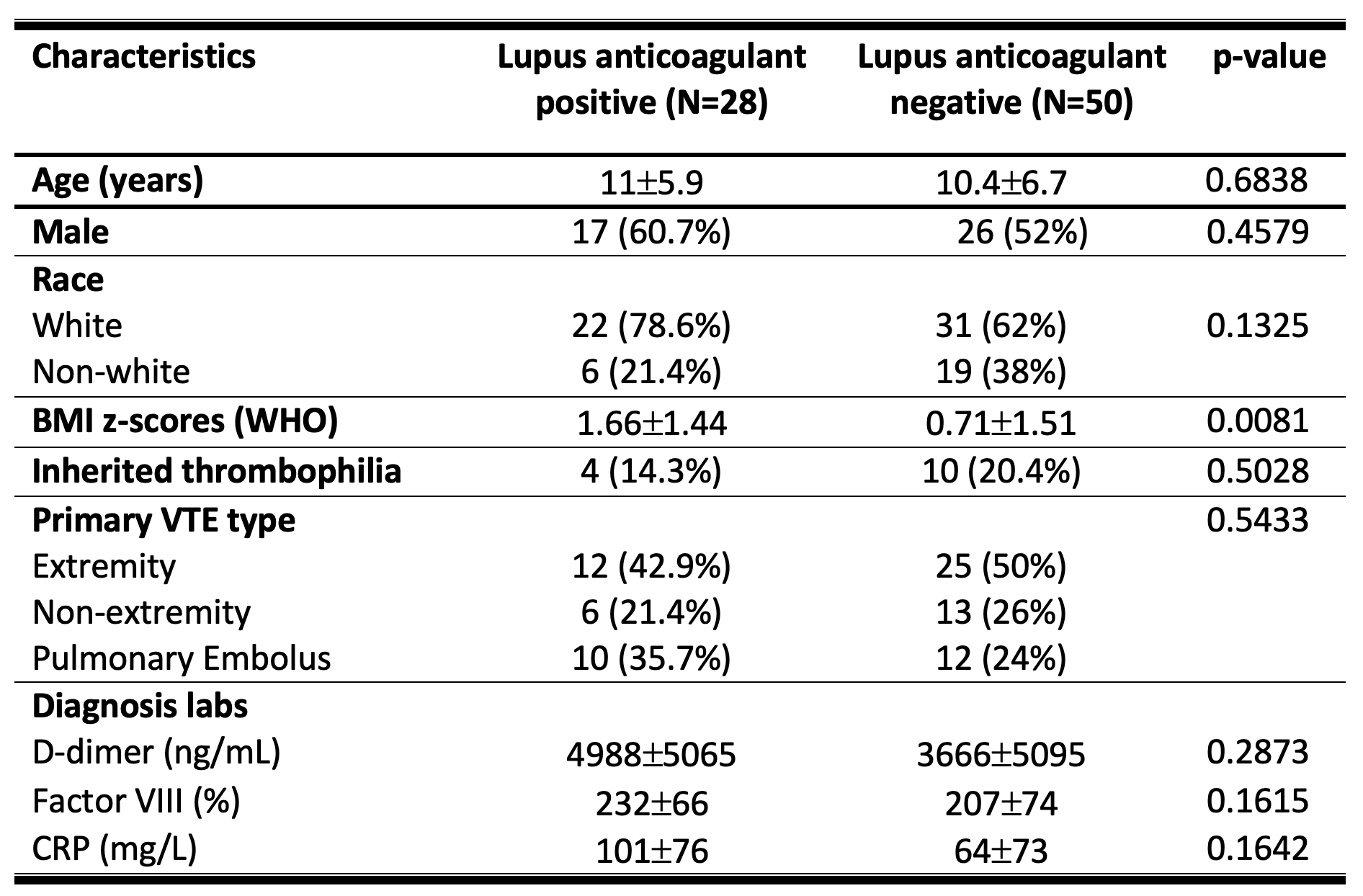 Table 1. Demographic Characteristics
Table 1. Demographic Characteristics
 Figure 1. Impact of LA positivity on the development of clinical outcomes
Figure 1. Impact of LA positivity on the development of clinical outcomes
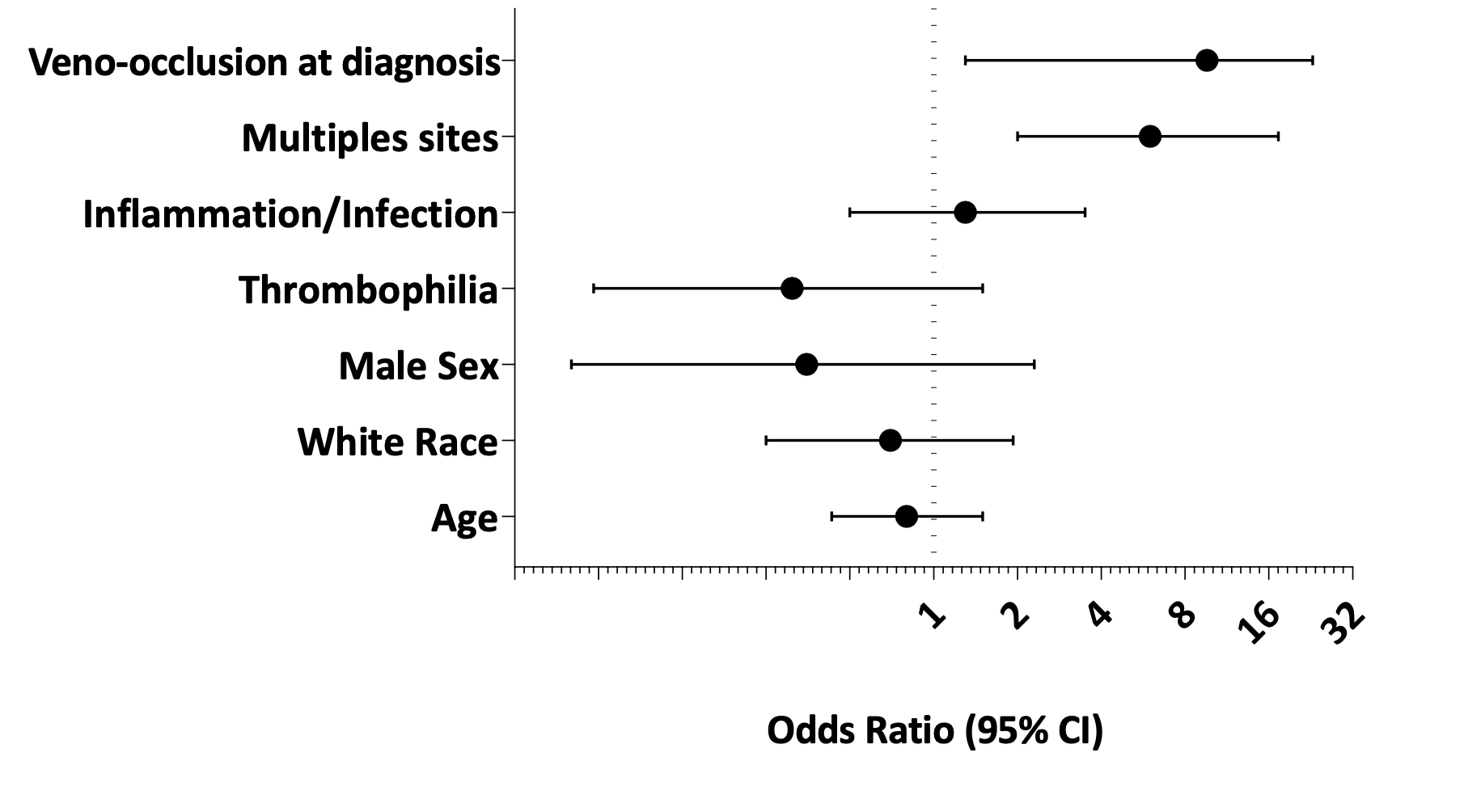 Figure 2. Predictors of composite clinical outcomes in LA positive patients
Figure 2. Predictors of composite clinical outcomes in LA positive patients
To cite this abstract in AMA style:
Sloan E, Zia A. Lupus Anticoagulant as a Predictor of Adverse Outcomes in Children with Venous Thromboembolism [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/lupus-anticoagulant-as-a-predictor-of-adverse-outcomes-in-children-with-venous-thromboembolism/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lupus-anticoagulant-as-a-predictor-of-adverse-outcomes-in-children-with-venous-thromboembolism/
