Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: The COVID19 pandemic necessitated practice changes throughout health systems worldwide. Our academic rheumatology practice rapidly adopted telehealth (telephone or video visits), with unknown consequences regarding providers’ time spent in the electronic health record (EHR) and ability to maintain patient care. We therefore analyzed changes in EHR utilization with telehealth implementation within our practice during COVID19.
Methods: Data were obtained using Slicer Dicer and Signal, analytic data tools in our EHR to evaluate practice patterns. We evaluated changes in the proportion of in-person versus telehealth visits, physician time spent per scheduled appointment in EHR activities (notes, orders, clinical review, and in-basket), and number of in-basket messages per day. Data were analyzed using descriptive statistics.
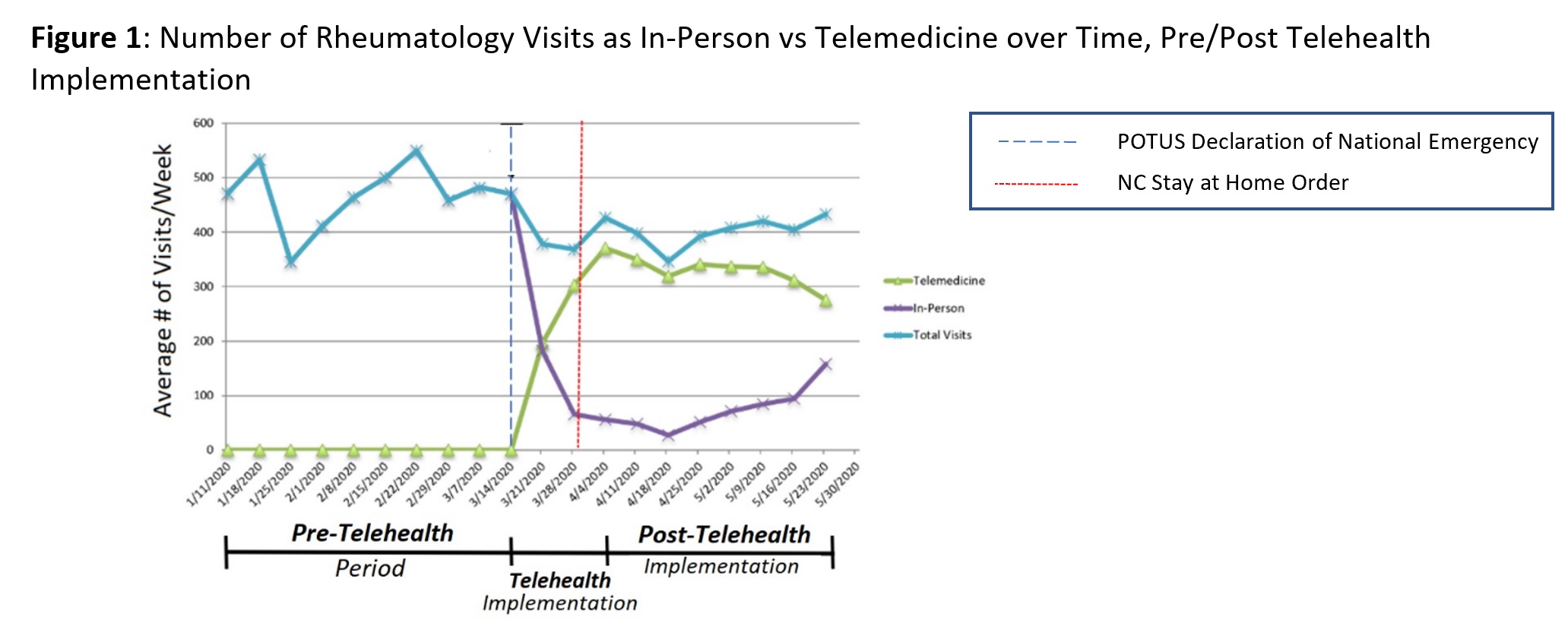
Results: In response to the COVID-19 pandemic and national emergency declared on March 13, 2020, our practice (28 providers) began transitioning to telehealth on March 15. During the Pre-Telehealth Period (Jan 5 – Mar 14), there was an average of 468 in-person visits/week and 0 telehealth visits. During the Telehealth Implementation Period (Mar 15 – Apr 4), the proportion of total visits completed via Telehealth expanded rapidly: 52% in Week 1, 82% in Week 2, and 87% in Week 3 (Figure 1). Post-Telehealth Implementation (Apr 4 – May 23), telehealth visits peaked at 92% (Apr 18) followed by a gradual decline to 63% (May 23). The average number of total visits per week in the Post-Telehealth Implementation Period was 400, a 15% decline compared with the Pre-Telehealth Period.
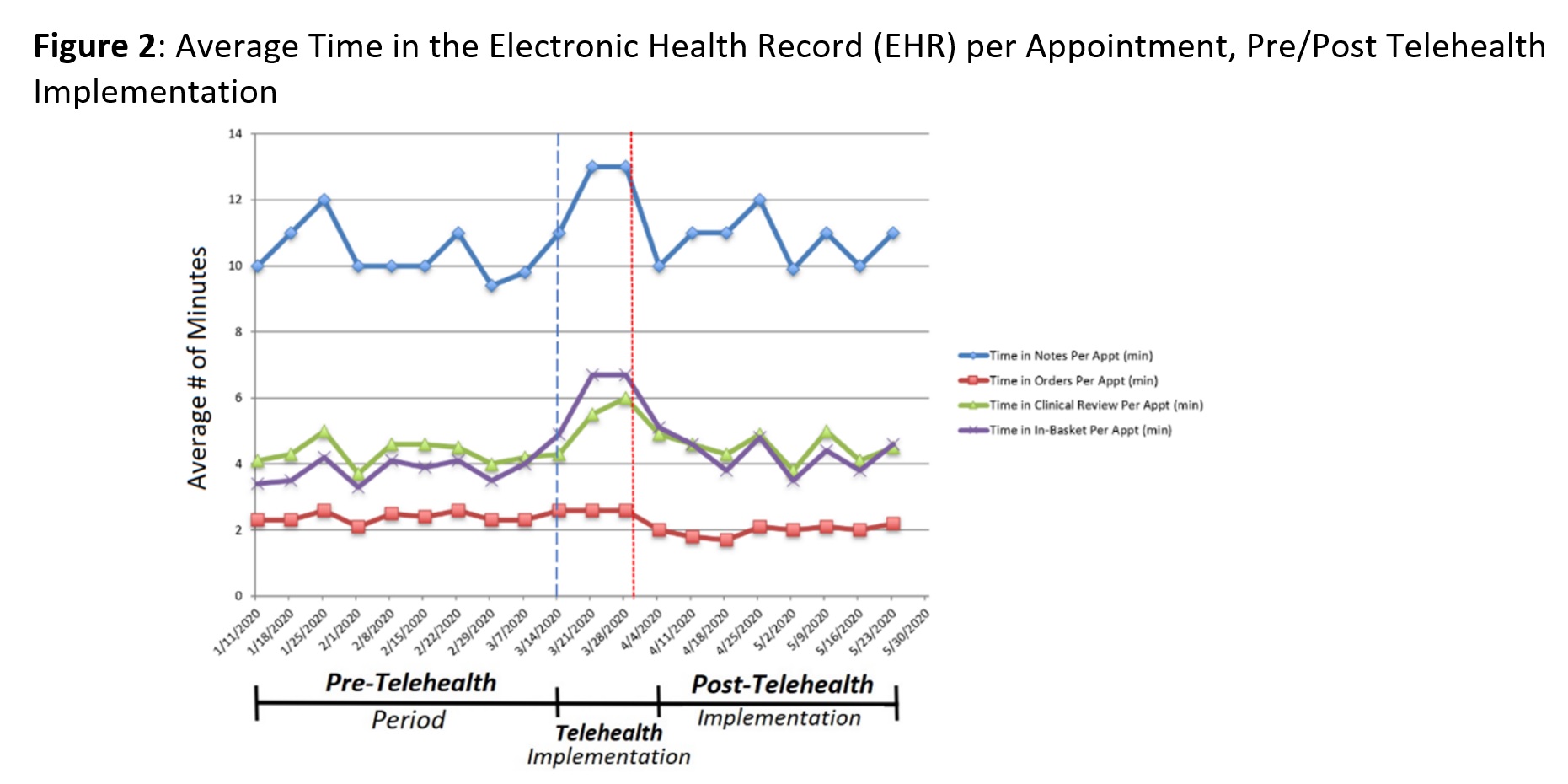
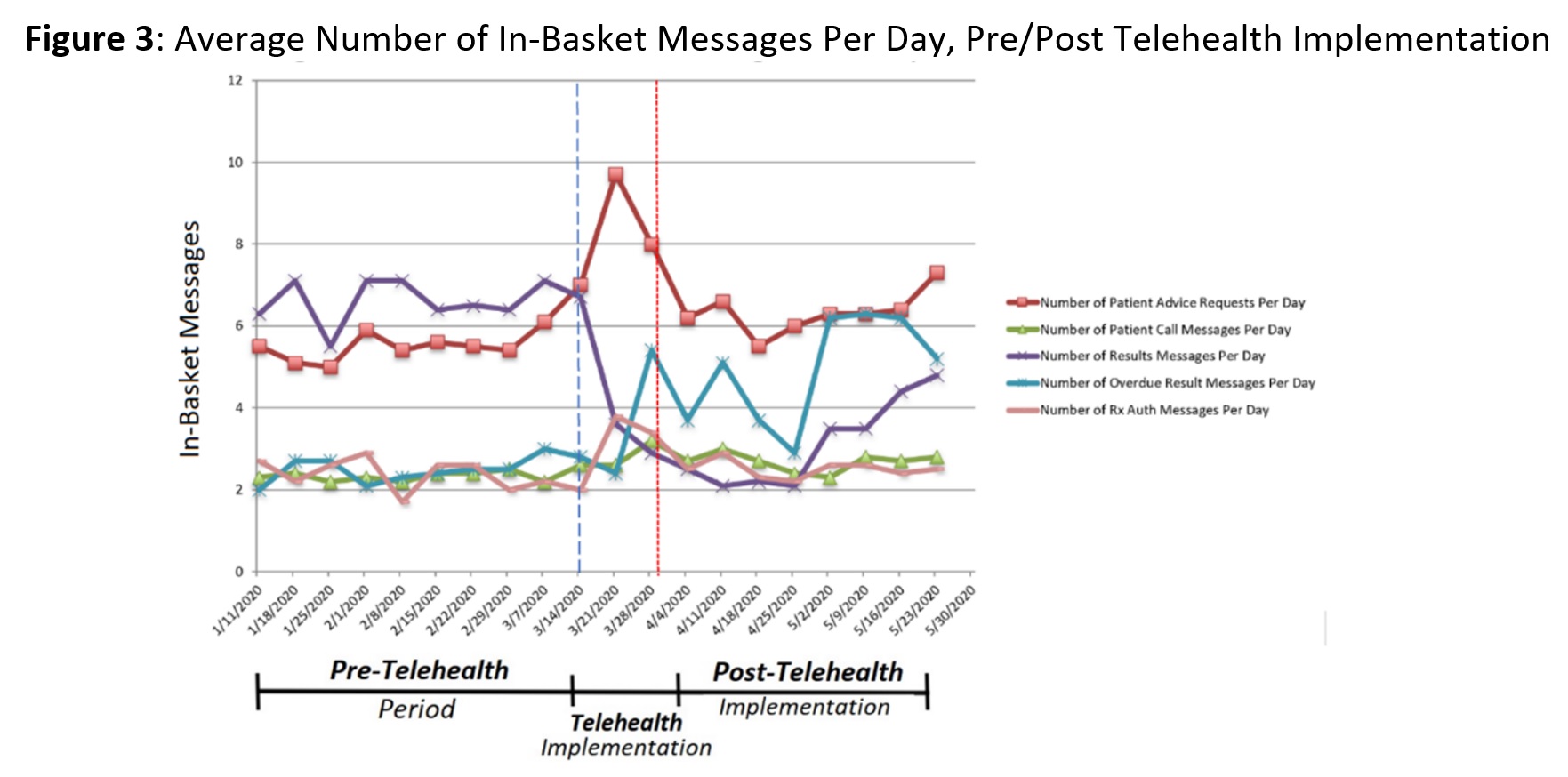
During the Telehealth Implementation Period, we observed increased average EHR time per appointment in notes, in-basket and clinical review while time in orders remained stable (Figure 2). The average number of in-basket messages/day for patient advice requests, prescription authorization requests, and overdue lab result messages all increased (Figure 3). During the Post-Telehealth Implementation Period, patient advice and prescription authorization requests approached Pre-Telehealth levels, with a delayed increase in overdue lab result messages/day (Figure 3).
Conclusion: During the COVID-19 pandemic, our practice’s clinical volume only declined by 15% by rapidly shifting from all in-person visits to 87% of visits ( >300/week) by Telehealth over 3 weeks. This transition required more time spent in multiple EHR activities and more in-basket requests (especially patient advice and prescription requests) during telehealth implementation. We hypothesize that this reflects increased time spent coordinating care, answering patient questions about COVID19, and refilling hydroxychloroquine and other DMARDs in advance of potential shortages. Subsequently, our overall EHR utilization returned near baseline, suggesting sustainability of this practice pattern. During telehealth implementation, we observed a decrease in result messages per day, highlighting the difficulty of obtaining medication toxicity monitoring and other laboratory testing during telehealth. We plan to continue monitoring this data with future shifts in practice.
To cite this abstract in AMA style:
Maheswaranathan M, Chu P, Johannemann A, Clowse M, Criscione-Schreiber L, Leverenz D. Impact of Telehealth Implementation on Practice Patterns and Electronic Health Record Utilization During COVID19 [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/impact-of-telehealth-implementation-on-practice-patterns-and-electronic-health-record-utilization-during-covid19/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-telehealth-implementation-on-practice-patterns-and-electronic-health-record-utilization-during-covid19/