Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Granulomatosis with polyangiitis (GPA) is a rare and life-threatening autoimmune disease. Due to the extremely low prevalence of GPA, monitoring of clinical characteristics and outcomes is critical. The objective of this study was to analyze the clinical presentations and follow-up results of patients diagnosed with the GPA at a national referral center in Iran.
Methods: Between 2012 and 2020, all consecutive GPA-diagnosed patients at Tehran University of Medical Sciences (Amir A’lam Hospital) were included. All patients fulfilled the 1990 ACR criteria and/or revised Chapel Hill nomenclature for GPA. Patients’ demographic information, laboratory findings, and clinicopathological manifestations were retrospectively recorded in the GPA registry system.
Results: Overall, 220 GPA patients, including 112 (50.9%) men and 108 (49.1%) women, with the mean age of 44.4 ± 15.9 years, were diagnosed. The mean follow-up time was 24.6 months. The mean interval between disease onset and diagnosis was 23.6 months (ranged 6-300). Regarding clinical manifestation at diagnosis, ear nose throat (ENT) (99.5%), pulmonary (76.8%), and renal (46.8%) were the most commonly involved organs (Table 1). Sera positivity for anti-proteinase 3 (PR3)-ANCA and myeloperoxidase (MPO)-ANCA were found in 138 (63.3%) and 29 (13.3%) patients, respectively. Histologic data obtained from 140 patients, revealed the classical triad of vasculitis, necrosis, and granulomatous inflammation in 29 specimens (19%). Regarding inflammatory serological markers, high levels of CRP ( >10 mg/L) was observed in 137 (62.8%) and high ESR levels ( >30 mm/h) in 122 (55.9%) patients (Table 2). Regarding disease severity, the mean BVAS/WG and PGA scores at the time of diagnosis were calculated as 9.5 ± 4.3 and 5.9 ± 1.8, respectively. Accordingly, based on the BVAS/WG classification, 141 (64%) patients fell into severe and 79 (36%) in limited disease activity categories. Based on the last recorded follow-up, ENT, pulmonary, and renal were increased to 100%, 85.9%, and 56.8%, respectively. Among 103 patients with a minimum follow-up of 24 months, 161 relapses occurred (mean relapse count for each patient: 1.56). Sixty-nine (31.3 %) patients expired during the follow-up period, 46 (66.6 %) less than 1 year, 16 (23.1 %) between 1 to 5 years and 7 (10.1 %) after 5 years post-diagnosis. There was a significant change in the main causes of death in the study timeframe (p-value = 0.001). During the first year after diagnosis of GPA, the most common cause of death was active vasculitis (19 Of 46; 41.3%), whereas from years 1 to 5 after the diagnosis, the most frequent cause was cardiovascular (CVD) disease (8 Of 16; 50%), and from years 5 to 10, malignancy and CVD were the most common causes (3 Of 7; 42.8% each).
Conclusion: GPA has a progressive nature, which, despite the continuous treatment, it moves to a more severe form. GPA-related death might occur either as the results of disease directly (organs involvement) or long-term side-effects related to treatments (e.g., malignancy). Thereby, early diagnosis of disease, regular follow-up, and using non-carcinogenic therapies (e.g., rituximab instead of cyclophosphamide) could be useful to decrease disease severity and mortality rate.
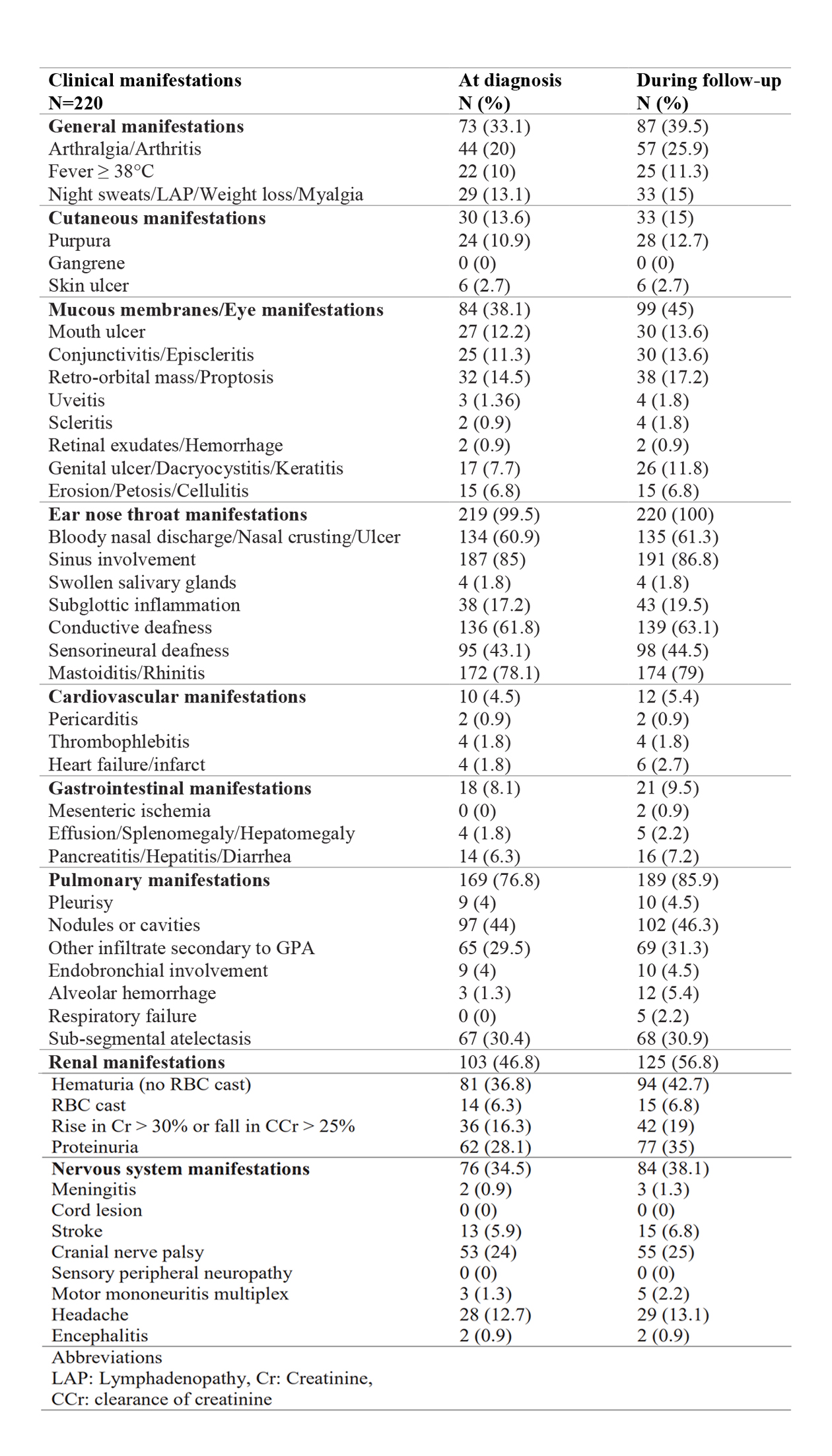 Table 1. Clinical manifestations at diagnosis and during follow up obtained from a cohort of 220 GPA patients from 2012 to 2020 at a national referral center
Table 1. Clinical manifestations at diagnosis and during follow up obtained from a cohort of 220 GPA patients from 2012 to 2020 at a national referral center
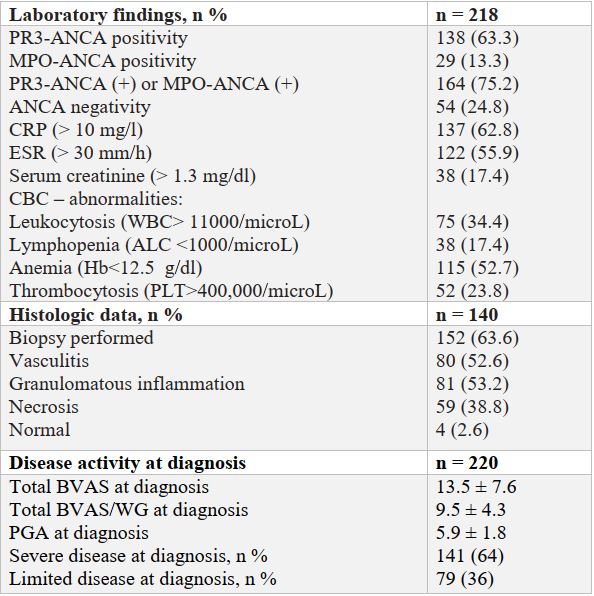 Table 2. Patients’ laboratory and histological findings and disease activity at diagnosis
Table 2. Patients’ laboratory and histological findings and disease activity at diagnosis
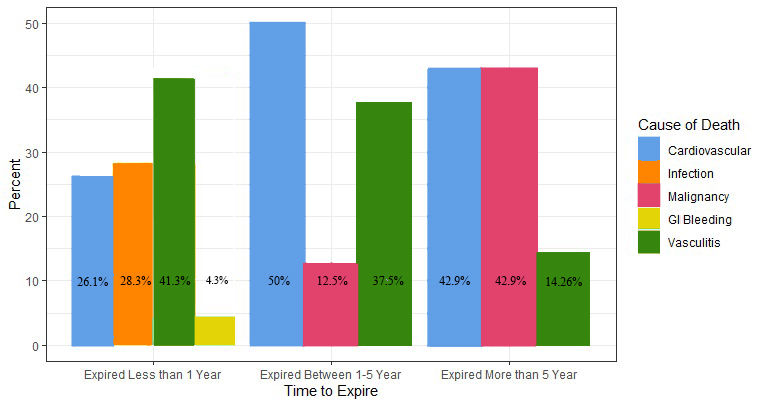 Figure 1. The causes of death during study timeframe.
Figure 1. The causes of death during study timeframe.
To cite this abstract in AMA style:
Jazayeri S, Kianifar F, Alesaeidi S, Tavakolpour S, Teimourpour A, Dabiri S. Clinical Presentations and Follow-up Results of Granulomatosis with Polyangiitis: An Analysis of 8 Years Clinical Experience with 220 Patients from a National Referral Center [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/clinical-presentations-and-follow-up-results-of-granulomatosis-with-polyangiitis-an-analysis-of-8-years-clinical-experience-with-220-patients-from-a-national-referral-center/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-presentations-and-follow-up-results-of-granulomatosis-with-polyangiitis-an-analysis-of-8-years-clinical-experience-with-220-patients-from-a-national-referral-center/
