Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Several systemic autoimmune rheumatic diseases have been shown to increase coronary artery disease (CAD) risk, notable rheumatoid arthritis and systemic lupus erythematosus. However, data on the risk of systemic sclerosis (SSc) and CAD is unclear. Although not a common finding, some studies have shown an increased prevalence of CAD in SSc patients. This has been attributed to the underlying vascular abnormalities. Other studies have failed to show a significant difference in the prevalence of CAD compared to the general population. The primary aim of this study was to assess the outcomes of SSc patients who were primarily hospitalized for acute myocardial infarction (AMI) from a nationally representative sample.
Methods: We used data from the National Inpatient Sample (NIS) for the period of 2016 to 2017 for adult AMI hospitalizations as a primary diagnosis and systemic sclerosis as a secondary diagnosis using ICD-10 codes. The proportion who met ACR classification criteria and disease activity status cannot be determined within the NIS database. We used STATA 15 for the data analysis and multivariate logistic regression to calculate the adjusted odds ratios for inpatient mortality in AMI hospitalizations.
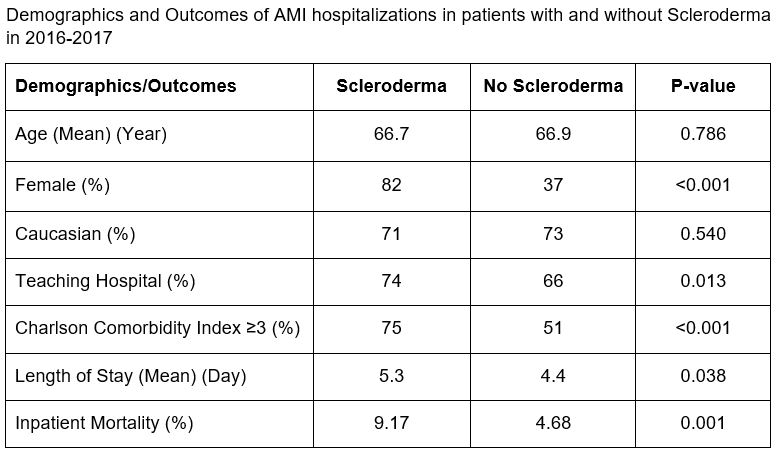
Results: We identified a total of 1,305,889 AMI hospitalizations between 2016 and 2017 of which 1,145 (0.08%) had a diagnosis of SSc. Compared to the non-SSc group, patients with SSc were predominantly female (82.1% vs. 37.9%; p< 0.001). There was no statistically significant difference in the age between two groups of patients.
Compared to non-SSc hospitalizations with AMI, SSc hospitalizations had a higher unadjusted inpatient mortality rate (9.17% vs. 4.68%; p=0.001). After adjusting for gender, age, race, household income, hospital location, hospital teaching status, hospital bed size and Charlson Comorbidity Index, the odds ratio (OR) for hospital mortality due to AMI in SSC patients was higher and statistically significant (aOR=2.02; 95% CI= 1.28-3.19; p=0.002) compared to the non-SSc group. Length of stay was significantly longer in patients with SSc (5.3 vs 4.4 days; p=0.038).
Conclusion: In our study, unadjusted and adjusted inpatient mortality in SSc patients primarily hospitalized for AMI was higher than non-SSc patients with an adjusted odds ratio of 2.02. This finding indicates that patients with SSc may have worse outcomes for cardiovascular events when admitted for AMI. Further study in optimizing cardiovascular risk factors in SSc patients is paramount in order to minimize their cardiac morbidity and mortality.
To cite this abstract in AMA style:
Vafa A, Behnamfar O, Lin Y. Outcomes of Systemic Sclerosis Patients Who Were Primarily Admitted for Acute Myocardial Infarction from 2016 to 2017: Insights from the National Inpatient Sample [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/outcomes-of-systemic-sclerosis-patients-who-were-primarily-admitted-for-acute-myocardial-infarction-from-2016-to-2017-insights-from-the-national-inpatient-sample/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-of-systemic-sclerosis-patients-who-were-primarily-admitted-for-acute-myocardial-infarction-from-2016-to-2017-insights-from-the-national-inpatient-sample/