Session Information
Date: Sunday, November 8, 2020
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The COVID-19 pandemic has quickly emerged as the most challenging global health crisis in a generation. Affecting initially China, New York City (NYC) quickly became the epicenter. Data has been scarce for populations at the highest risk of infection, most notably immunosuppressed patients with underlying chronic inflammatory diseases or chronic use of anti-cytokine biologics and/or other immunomodulatory therapies. We aimed to characterize the hospitalization and death rates among patients with inflammatory arthritis (IA; rheumatoid arthritis and spondyloarthritis) affected by COVID-19 and to analyze the associations between comorbidities and immunomodulatory medications and infection outcomes.
Methods: Recruitment stemmed from a larger NYU Langone Health study, namely Web-based Assessment of Autoimmune, Immune-Mediated, and Rheumatic Patients during the COVID-19 Pandemic (WARCOV). WARCOV is a prospective cohort of patients with established diagnosis of immune mediated inflammatory disease. Participants were referred from 46 NYU affiliated providers throughout NYC. Clinical, demographic, maintenance treatment, and disease course data and outcomes of individuals with IA with symptomatic COVID-19 were prospectively assessed via web-based questionnaire, individual phone calls, and electronic medical record review. Baseline characteristics and medication use were summarized for hospitalized and ambulatory patients, and outcomes were compared for each medication class using multivariable logistic regression.
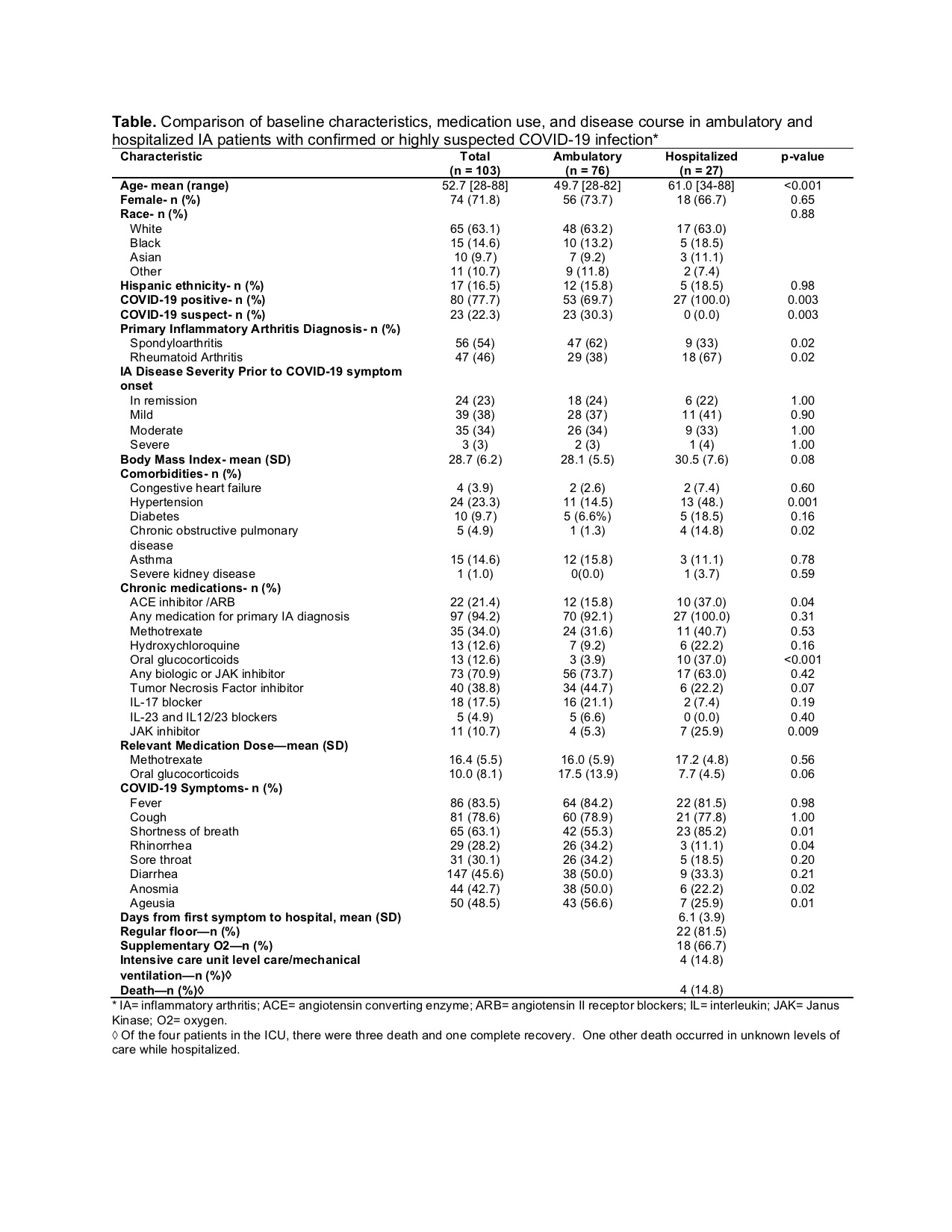
Results: A total of 103 patients with IA were included in the study (n=80 confirmed and n=23 highly suspicious for COVID-19). 26% of participants required hospitalization, and 4% died. Patients who warranted hospitalization were significantly more likely to be older (P< 0.001) and have comorbid hypertension (P=0.001) and chronic obstructive pulmonary disease (P=0.02) (Table). IA patients taking oral glucocorticoids had a higher likelihood of being admitted for COVID-19 (P< 0.001) while those on maintenance anti-cytokine biologic therapies did not. After adjusting for age and sex, hypertension and oral glucocorticoid use remained significant risk factors for hospitalization (OR 3.33, 95% CI 1.16 to 9.60, P=0.03 and OR 21.12, 95% CI 4.09 to 109.03, P<0.001, respectively). Patients with rheumatoid arthritis were more likely to be hospitalized compared to those with spondyloarthritis, but were also older and more likely to be on oral glucocorticoids.
Conclusion: In patients with underlying IA, COVID-19 outcomes were worse in patients receiving glucocorticoids but, importantly, not in patients on maintenance anti-cytokine therapy. As with non-IA patients, age and hypertension were also associated with hospitalization. However, given our limitations of a relatively small number of hospitalizations and likely confounding by indication, caution should be taken in the interpretation of these results. Further work, currently underway, is needed to better understand whether immunomodulatory therapies affect COVID-19 incidence and its natural history.
To cite this abstract in AMA style:
Haberman R, Castillo R, Chen A, Yan D, Ramirez D, Sekar V, Lesser R, Solomon G, Neimann A, Blank R, Izmirly P, Webster D, Ogdie A, Troxel A, Adhikari S, Scher J. COVID-19 in Patients with Inflammatory Arthritis: A Prospective Study on the Effects of Comorbidities and DMARDs on Clinical Outcomes [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/covid-19-in-patients-with-inflammatory-arthritis-a-prospective-study-on-the-effects-of-comorbidities-and-dmards-on-clinical-outcomes/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/covid-19-in-patients-with-inflammatory-arthritis-a-prospective-study-on-the-effects-of-comorbidities-and-dmards-on-clinical-outcomes/