Session Information
Date: Sunday, November 8, 2020
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients presenting with back pain and psoriasis, acute anterior uveitis (AAU), or inflammatory bowel disease (IBD), represent a high-risk population for the presence of axial spondyloarthritis (axSpA) but may remain undiagnosed for many years. Several referral strategies have been proposed aiming at pre-selecting patients with a high probability of having axSpA among the common condition of non-specific back pain in primary care. The Berlin criteria include inflammatory back pain (IBP), B27 and sacroiliitis by imaging. The ASAS modification excludes IBP as a mandatory entry item. The Dublin Evaluation Tool (DUET) restricted to AAU is based on joint pain, B27 and cutaneous psoriasis, but not on IBP. Validation of these algorithms in inception cohorts is limited.
We aimed to: (1) compare the performance of referral algorithms in an inception cohort of patients with extra-articular manifestations presenting to a rheumatologist with undiagnosed back pain, when tested against the final local rheumatologist; (2) determine whether different IBP criteria impact the performance of the algorithms.
Methods: The multicenter Screening for Axial Spondyloarthritis in Psoriasis, Iritis, and Colitis (SASPIC) Study at 11 sites is aimed at early detection of axial SpA in consecutive patients presenting with undiagnosed back pain to the rheumatologist. Consecutive patients ≤45 years of age with ≥3 months undiagnosed back pain with any one of psoriasis, AAU, or IBD undergo routine clinical evaluation by a rheumatologist for axSpA. The rheumatologist determines the presence or absence of axSpA at 3 consecutive stages: 1. After the clinical evaluation; 2. After the results of labs (B27, CRP) and radiography; 3. After the results of MRI evaluation. Final diagnosis by the rheumatologist was used as external standard to test the performance of the algorithms. We tested the following criteria for IBP in the algorithm: ASAS, Berlin, rheumatologist global for likelihood of IBP >5 (0-10 scale), and DUET in AAU.
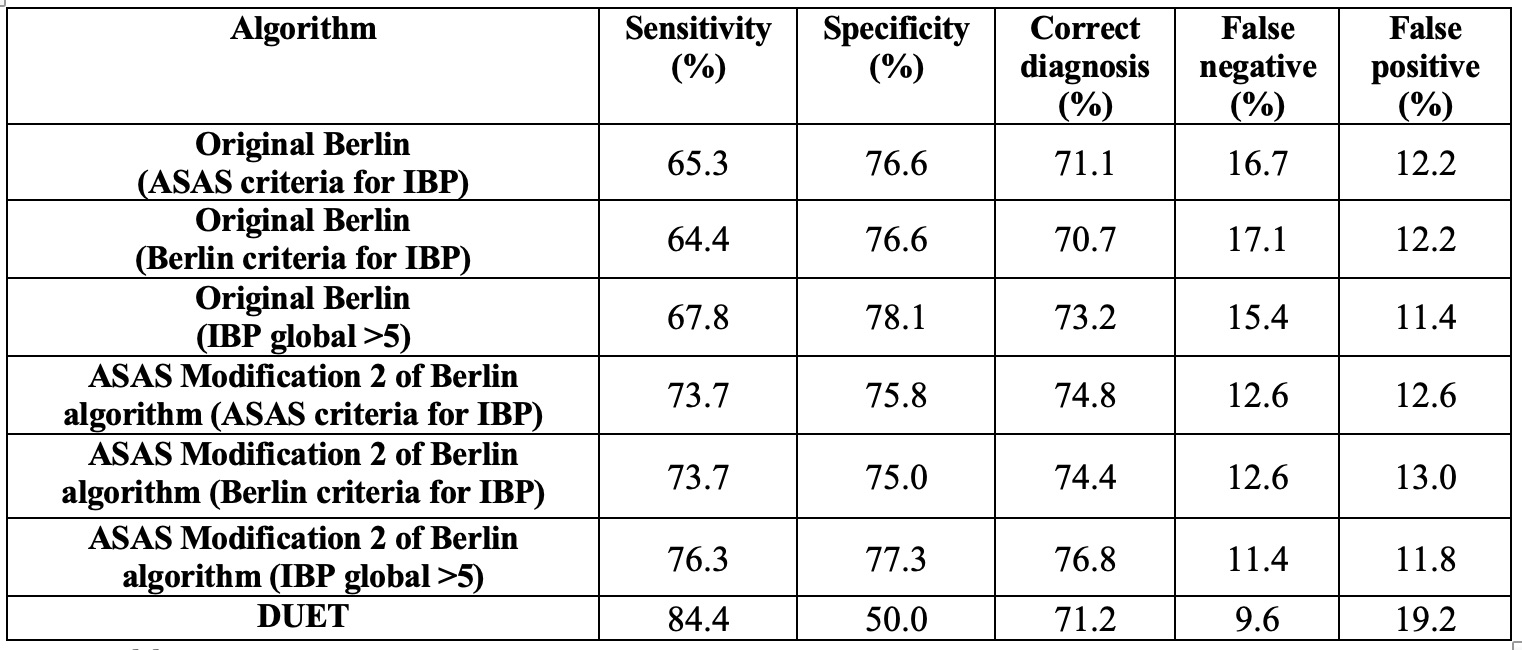
Results: 246 patients were recruited, 73 presented with AAU, 46 with psoriasis, and 127 with IBD. 47.6% were diagnosed with axSpA (68.5% B27-positive). The diagnosis of axSpA was established in 45.7%, 61.6%, and 40.2% of patients with psoriasis, AAU, and IBD, respectively. The performance of the ASAS-modification of the Berlin algorithm was superior to the original algorithm as reported previously3, primarily for enhanced sensitivity, and this was observed irrespective of the IBP criteria (Table 1). Conversely, the DUET algorithm in the subset of patients with AAU performed worse than previously reported1.
Conclusion: The ASAS modification of the Berlin algorithm showed the optimal balance between sensitivity and specificity and represented the preferred referral strategy for patients presenting with undiagnosed back pain and extra-articular features.
- Haroon M et al. Ann Rheum Dis 2015;74:1990
- Poddubnyy D et al. J Rheumatol 2011;38: 452
- Van den Berg R et al. Ann Rheum Dis 2013;72:1646
To cite this abstract in AMA style:
Weber U, Carmona R, Yeung J, Chan J, Martin L, Masetto A, Keeling S, Ziouzina O, Rohekar S, Dadashova R, Paschke J, Carapellucci A, Lambert R, Maksymowych W, Aydin S. Performance of Three Referral Algorithms for Diagnosing Axial Spondyloarthritis: Results from the Screening in Axial Spondyloarthritis for Psoriasis, Iritis, and Colitis Cohort [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/performance-of-three-referral-algorithms-for-diagnosing-axial-spondyloarthritis-results-from-the-screening-in-axial-spondyloarthritis-for-psoriasis-iritis-and-colitis-cohort/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/performance-of-three-referral-algorithms-for-diagnosing-axial-spondyloarthritis-results-from-the-screening-in-axial-spondyloarthritis-for-psoriasis-iritis-and-colitis-cohort/